Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
POLICY
STATEMENT
Approved April 2023
Ultrasound Guidelines:
Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in
Medicine
Revised April 2023,
June 2016 with current
title
Revised October 2008
Originally approved June
2001 titled “Emergency
Ultrasound Guidelines”
Sections
1. Introduction
2. Scope of Practice
3. Training and Proficiency
4. Hospital Credentialing and Privileging
5. Specialty Certification
6. Quality and Ultrasound (US) Management
7. Value and Reimbursement
8. Clinical US Leadership in Healthcare Systems
9. Future Issues
10. Conclusion
Tables
1. Emergency Medicine Ultrasound Definitions
Figures
1. ACEP 2023 Emergency US Scope of Practice
2. Pathways for Clinical US Training, Credentialing, and Incorporation
of New Applications
3. Clinical US Workflow
Appendices
1. Evidence for Core Emergency US Applications
2. Evidence for Advanced Emergency US Applications
3. Emergency US Learning Objectives
4. Recommendations for EM Residency EUS Education Program
5. Recommendations for EUS Course
6. US in UME - Medical School Rotation and Curriculum
ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 2 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
Section 1 – Introduction
Clinical ultrasound (CUS) has become an integral aspect of emergency care in the United States for over two
decades. Since the last update of these guidelines in 2016, the role of US has expanded throughout clinical
medicine. The wide breadth of recognized CUS applications offers both diagnostic and therapeutic benefits
to patients around the world. Benefits of bedside imaging with ultrasound include its relatively low cost, lack
of ionizing radiation, portability, and ease of use. Data have demonstrated that CUS can improve diagnostic
accuracy in numerous common clinical presentations, including dyspnea,
1
abdominal pain,
2
and joint
dislocations.
3
Ultrasound guidance has also been incorporated into bedside procedures, improving success
and decreasing inadvertent complications.
4-6
Emergency physicians have been leaders in innovation and education in the CUS space both nationally and
internationally. This has led to increased integration and improved standardization at the undergraduate,
postgraduate, and continuing medical education levels. Emergency medicine (EM) leaders have also
leveraged their extensive knowledge and teaching to educate other specialties seeking to enhance their
ultrasound training and expertise. Specifically, CUS curricula in undergraduate medical education is growing
exponentially due to the leadership and advocacy of emergency physicians, integrating CUS into the
education of the next generation of clinicians. In fact, CUS in EM residency training has been codified in the
Model of the Clinical Practice of Emergency Medicine, a joint policy collaboration between seven
organizations. Moreover, CUS fellowship has advanced with fellowships now eligible for accreditation by
the Emergency Ultrasound Fellowship Accreditation Council (EUFAC) and fellowship graduates being
recognized with certification as a focused practice designation by ABEM. Leaders in CUS have created the
foundation of a subspecialty of ultrasonography that provides the expertise for establishing clinical practice,
educating across the educational spectrum, and researching the wide range of applications. CUS leaders have
also become instrumental in bringing health care systems into the future by championing and often running
system-wide programs. As CUS continues to evolve and access to ultrasound machines becomes increasingly
widespread, it is critical to understand the current field and provide national guidelines to inform education
and practice. This guideline update is intended to provide a framework for new and established programs
utilizing CUS.
Section 2 -- Scope of Practice
CUS is the medical use of US technology for the bedside, clinical evaluation of acute or critical medical
conditions.
7
It is utilized for diagnosis of any emergency condition such as the resuscitation of the critically
ill patient, during guidance of procedures, and monitoring of certain pathologic states. CUS examinations are
typically performed and interpreted by emergency physicians or those under the supervision of emergency
physicians in the setting of the emergency department (ED) or a non-ED emergency setting hospital unit, out-
of-hospital, battlefield, space, urgent care, clinic, or remote or other settings). It may be performed as a single
examination, repeated serially due to clinical need or patient deterioration, or used for monitoring of
physiologic or pathologic changes.
In this document, CUS refers to US performed by emergency physicians or clinicians in the emergency
setting, while point-of-care ultrasound (POCUS) refers to a multidisciplinary field of US use by clinicians at
the point-of-care.
8
Table 1 summarizes relevant US definitions in CUS.
Other medical specialties may wish to use this document if they perform CUS in the manner described above.
However, guidelines which apply to US examinations or procedures performed by consultants, especially
consultative imaging in US laboratories or departments, or in alternative settings may not be applicable to
emergency physicians.

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 3 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
Emergency US (EUS) is an emergency medicine procedure, and should not be considered in conflict with
exclusive “imaging” contracts that may be in place with consultative US practices. In addition, emergency
US should be reimbursed as a separate billable procedure.
9
(See Section 7- Value and Reimbursement)
CUS is a separate entity distinct from the physical examination that adds anatomic, functional, and
physiologic information to the care of the acutely-ill patient.
10
It provides clinically significant data not
obtainable by inspection, palpation, auscultation, or other components of the physical examination.
11
US used
in this clinical context is also not equivalent to use in the training of medical students and other clinicians in
training looking to improve their understanding of anatomic and physiologic relationships of organ systems.
CUS can be classified into the following functional clinical categories:
1. Resuscitative: US use as directly related to an acute resuscitation
2. Diagnostic: US utilized in an emergent diagnostic imaging capacity
3. Symptom or sign-based: US used in a clinical pathway based upon the patient’s symptom or sign (eg,
shortness of breath)
4. Procedure guidance: US used as an aid to guide a procedure
5. Therapeutic and Monitoring: US use in therapeutics or in physiological monitoring
Within these broad functional categories of use, 15 core emergency US applications have been identified as
Aorta, Bowel, Cardiac/Hemodynamic assessment, Deep Vein Thrombosis (DVT), Hepatobiliary,
Musculoskeletal (MSK), Ocular, Pregnancy, Procedural Guidance, Skin and Soft-tissue, Testicular,
Thoracic/Airway, Trauma, Ultrasound-Guided Nerve Blocks, and Urinary Tract. Evidence for these core
applications may be found in Appendix 1. The criteria for a core application are widespread use, significant
evidence base, uniqueness in diagnosis or decision-making, importance in primary emergency diagnosis and
patient care, or technological advance.
Alternatively, symptom and sign based US pathways, such as Shock or Dyspnea, may be considered an
integrated application based on the skills required in the pathway. In such pathways, applications may be
mixed and utilized in a format and order that maximizes medical decision-making, outcomes, efficiency and
patient safety tailored to the setting, resources, and patient characteristics. See Figure 1.
Emergency physicians should have basic education in US physics, knobology, instrumentation procedural
guidance, and Focused Assessment with Sonography in Trauma (FAST) as part of EM practice. It is not
mandatory that every clinician performing emergency US examinations utilize or be expert in each core
application, but it is understood that each core application is incorporated into common emergency US
practice nationwide. The descriptions of these examinations may be found in the ACEP policy, Emergency
Ultrasound Imaging Criteria Compendium.
12
Many other US applications or advanced uses of these
applications may be used by emergency physicians. Their non-inclusion as a core application does not
diminish their importance in practice nor imply that emergency physicians are unable to use them in patient
care.
Each EUS application represents a clinical bedside skill that can be of great advantage in a variety of
emergency patient care settings. In classifying an emergency US, a single application may appear in more
than one category and clinical setting. For example, a focused cardiac US may be utilized to identify a
pericardial effusion in the diagnosis of an enlarged heart on chest x-ray. The focused cardiac US may be
utilized in a cardiac resuscitation setting to differentiate true pulseless electrical activity from profound
hypovolemia. The focused cardiac US can be used to monitor the heart during resuscitation in response to
fluids or medications. If the patient is in cardiac tamponade, the cardiac US can also be used to guide a
pericardiocentesis. In addition, the same focused cardiac study can be combined with one or more additional

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 4 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
emergency US types, such as the focused abdominal, the focused aortic or the focused chest/thoracic US, into
a clinical algorithm for an undifferentiated hypotensive patient. See Figure 1.
Ultrasound guidance provides added safety to a wide variety of procedures ranging from vascular access (eg,
central venous access) to drainage procedures (eg, thoracentesis pericardiocentesis, paracentesis,
arthrocentesis) to localization procedures like US guided nerve blocks. These procedures may provide
additional benefits by increasing patient safety and helping alleviate acute pain.
Other US applications are performed by emergency physicians, and may be integrated depending on the
setting, training, and needs of that particular ED or EM group.
Other Settings or Populations
Pediatrics. CUS is a particularly advantageous diagnostic tool in the management of pediatric patients, in
whom radiation exposure is a significant concern. CUS applications such as musculoskeletal evaluation for
certain fractures (rib, forearm, skull), and lung for pneumonia may be more advantageous in children than in
adults due to smaller patient size and density.
13
US can be associated with increased procedural success and
patient safety, and decreased length of stay.
14,15
While most US modalities in the pediatric arena are the same
as in adult patients (the EFAST exam for trauma, procedural guidance), other modalities are unique to the
pediatric population such as in suspected pyloric stenosis and intussusception, or in the child with hip pain or
a limp).
16-18
Mostly recently, EUS has been formally incorporated into Pediatric EM fellowship training.
19,20
Critical Care. CUS core applications are being integrated into cardiopulmonary resuscitations and non-
invasive hemodynamic monitoring into critical care scenarios.
21,22
Dual-trained physicians in emergency
medicine and critical care are leading the application, education, and research of US for critically ill patients,
and have significant leadership in advancing US concepts in multidisciplinary critical care practice. Advanced
cardiopulmonary US application are being integrated into critical care practice.
Prehospital. There is increasing evidence that CUS has an increasing role in out-of-hospital emergency
care.
23,24
Challenges to the widespread implementation of out-of-hospital US include significant training and
equipment requirements, and the need for oversight and quality assurance. Studies focusing on patient
outcomes need to be conducted to further define the role of out-of-hospital CUS and to identify settings where
the benefit to the patient justifies the investment of resources necessary to implement such a program.
25
International arena including field, remote, rural, global public health and disaster situations. US has
become the primary initial imaging modality in disaster care.
26-30
US can direct and optimize patient care in
natural disasters such as tsunami, hurricane, famine or man-made disasters such as battlefield or refugee
camps. US allows for imaging in remote locations such as rural areas, developing countries, or small villages
which often do not have other imaging options (eg, x-ray, CT, MRI), unreliable electrical supplies, and less
experienced clinicians. US in outer space is often the only imaging modality for space exploration and
missions.
31,32
Ultrasound has also been used in remote settings such as international exploration, mountain
base camps, and cruise ships.
23
The increasing portability of US machines and development of handheld
devices with improving image resolution has expanded the use of emergent imaging in such settings.
Military and Tactical. The military has embraced the utilization of US technology in austere battlefield
environments.
33,34
It is now routine for combat support hospitals as well as forward surgical teams to deploy
with next generation portable ultrasonography equipment. Clinical ultrasonography is often used to inform
decisions on mobilization of casualties to higher echelons of care and justify use of limited resources. Within
the last decade, emergency physicians at academic military medical centers have expanded ultrasonography
training to clinical personnel who practice in close proximity to the point of injury, such as combat medics,
ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 5 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
special operations forces, physician assistants, and nurse practitioners.
35
The overarching goal of these
training programs is to create a generation of competent clinical sonologists capable of practicing “good
medicine in bad places.” The military is pursuing telemedicine-enabled US applications, automated US
interpretation capabilities, and extension of clinical ultrasonography in additional areas of operation, such as
critical care air evacuation platforms.
36
Section 3 – Training and Proficiency
Training in CUS often begins today in undergraduate medical education (UME) where students first learn
and practice the basics of sonography as part of their anatomy, pathophysiology, and physical exam
coursework.
37
During Graduate Medical Education (GME), clinicians increasingly learn to utilize CUS
applications specific to their specialty and practice environment.
38-40
Finally, clinicians continue to learn
evolving applications and new technologies through decades of practice.
41
Competency and Curriculum Recommendations
Competency in CUS requires the progressive development and application of increasingly sophisticated
knowledge and psychomotor skills.
42,43
First, the clinician needs to recognize the indications and
contraindications. Next, the clinician must be able to acquire adequate images. This begins with an
understanding of basic US physics, translated into the skills needed to operate the US system correctly
(knobology), while performing CUS application protocols on patients presenting with different conditions
and body habitus. Simultaneous with image acquisition, the clinician needs to interpret the imaging by
distinguishing normal anatomy, common variants, as well as a range of pathology from obvious to subtle.
Finally, the clinician must be able to integrate EUS exam findings into their medical decision-making.
Ultimately, this integration includes detailed knowledge of each particular exam’s accuracy, as well as proper
documentation for the medical record, credentialing, quality assurance, and reimbursement.
Given the continual advances in CUS, designing and implementing a comprehensive yet efficient curriculum
for diverse learners requires considerable faculty expertise, dedicated non-clinical time, and ongoing
department support. These updated guidelines continue to provide the learning objectives (See Appendix 2),
educational methods, and assessment measures for a EUS residency or practice-based curriculum.
Evolving Educational Methods
Accelerated by necessity during the COVID-19 pandemic, innovative educational methods increasingly
supplement more traditional education methods in EUS training.
44
Free open-access medical (FOAM)
education, including carefully curated narrated lectures, podcasts and blogs, help educators create an engaging
flipped clinical classroom.
45-48
For the trainee, asynchronous learning provides the opportunity to review
required knowledge on-demand and at their own pace. For teachers, less time may be spent providing
recurring didactics and more time dedicated to higher-level tasks such as teaching psychomotor skills and
integration of exam findings into patient and ED management.
Similar to knowledge learning, there are new educational methods to teach the required psychomotor skills
of EUS. The primary educational method continues to be small group hands-on training in the ED with CUS
faculty, followed by supervised examination performance during clinical work, with timely quality assurance
review and feedback. Simulation continues to play an important role as both an educational method and
assessment measure.
43,44,49,50
Investigators have demonstrated that simulation results in equivalent image
acquisition, interpretation, and operator confidence in comparison to traditional hands-on training. Simulation
provides the opportunity for deliberate practice of a new skill in a safe environment prior to actual clinical
performance. The use of simulation for deliberate practice improves the success rate of invasive procedures

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 6 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
and reduces patient complications. Additionally, simulation has the potential to expose trainees to a wider
spectrum of pathology and common variants than typically encountered during a POCUS rotation. Blended
learning created by the flipped classroom, live instructor training, and simulation provide the opportunity for
self-directed learning, deliberate practice and mastery learning.
51-53
Furthermore, gamification provides the
opportunity to actively engage learners while assessing and ultimately teaching clinical ultrasound knowledge
and skills.
54,55
Documenting Experience and Demonstrating Proficiency
Traditional set number benchmarks for procedural training in medical education have historically provided a
convenient method for documenting the performance of a reasonable number of exams needed for a trainee
to develop competency.
43
However, learning curves vary by trainee and application. Individuals learn the
required knowledge and psychomotor skills at their own unique pace. Supervision, opportunities to practice
different applications, and encounter pathology also likewise differ across departments.
Therefore, additional assessment measures need to be utilized in addition to set number benchmarks.
43,56
Recommended methods include the following: real-time supervision during clinical EUS, weekly quality
assurance (QA) image review sessions, ongoing individual QA image review exam feedback, standardized
knowledge assessments, small group Observed Structured Clinical Examinations (OSCEs), one-on-one
standardized direct observation tools (SDOTs), and simulation assessments.
57
Ideally these assessment
measures are completed both at the beginning and the end of a training period. Initial assessment measures
identify each trainee’s unique needs, providing the opportunity to modify a local curriculum as needed to
create more individualized learning plans. Final assessment measures demonstrate current trainee competency
and future learning needs, identify opportunities for curriculum improvement, and ideally are supported by
patient outcomes.
56
Trainees should complete a benchmark of 25-50 quality-reviewed exams in a particular application. Any
individual clinician’s learning curve may plateau below or above a set number benchmark for competency.
With continued deliberate practice, proficiency will continue to slowly improve along the asymptotic line of
expertise throughout a clinician’s career.
58
Previously learned knowledge and psychomotor skills will often
facilitate the learning and performance of new applications. For example, experience with FAST provides a
springboard application to learning the genitourinary, transabdominal pelvic, and resuscitative clinical
ultrasound applications.
Overall EUS trainees should complete a minimum benchmark of 150-300 total clinical US exams
depending on the number of applications being utilized. For example, an academic department regularly
performing greater than six applications may require residents to complete more than 150 exams, while a
community ED with practicing physicians just beginning to incorporate EUS with FAST and vascular access
may initially require less.
If alternative techniques are being used for an application, for example an endocavitary probe in early
pregnancy evaluation, the minimum for that application should include substantial experience in that
alternative technique. Trainees should complete a minimum of 10-15 examinations in the alternative
technique during the completion of the 25-50 exams, since learning to properly interpret the anatomy and
pathology occurs with each technique taught in a particular application.
Procedural US applications require fewer exams given prior knowledge, psychomotor skills, and clinical
experience with the traditional landmark-based techniques. Trainees should complete five quality reviewed
US-guided procedure exams or a learning module on an US-guided procedure task trainer.

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 7 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
Training exams need to include clinical and simulated patients with different conditions and body types.
Exams may be completed in different settings including clinical and educational patients in the ED, live
models at EUS courses, utilizing US simulators, and in other clinical environments. In-person supervision is
optimal during introductory education but is not required for residency or credentialing examinations after
initial didactic and supervised skills training. Evolving technologies now create the opportunity for remote
supervision and feedback even in resource-limited settings.
59-61
Abnormal or otherwise positive scans need to
be included during the completion of training exams used to meet credentialing requirements. When
pathology is not encountered during patient care, common variants and pathologic findings need to be
reviewed during QA or other educational sessions.
During benchmark completion (credentialing phase), all EUS exams should be quality reviewed for technique
and accuracy by EUS faculty. Alternatively, an EUS training portfolio of exam images and results may be
compared to other diagnostic studies and clinical outcomes in departments where EUS faculty are not yet
available. After initial training, continued quality assurance of EUS exams is recommended for a proportion
(5-10%) of ongoing exams to document continued competency. Secure online systems facilitate image review
and QA feedback, while also improving workflow, utilization, documentation, and reimbursement.
62
Training Pathways
There are two recommended pathways for clinicians to become proficient in EUS. See Figure 2. The majority
of emergency physicians today receive EUS training as part of an ACGME-approved EM residency. A second
practice-based pathway is provided for practicing EM physicians and other clinicians who did not receive
training during residency.
These updated EUS guidelines continue to provide the learning objectives, educational methods and
assessment measures for either pathway. Learning objectives for each application are described in Appendix
3.
Residency Based Pathway
EUS has been considered a fundamental component of emergency medicine training for over two decades.
63,64
The ACGME mandates procedural competency in EUS for all EM residents as it is a “skill integral to the
practice of Emergency Medicine.” Although the ACGME EM Milestones 2.0 project now includes ultrasound
within Patient Care Milestone eight, ABEM is currently working with emergency POCUS leaders to better
delineate diagnostic and procedural ultrasound withing the Emergency Medicine Model of Clinical Practice.
65
Appendix 4 provides recommendations for EM residency EUS education.
Upon completion of residency training, emergency medicine residents should be provided with a standardized
EM Resident EUS credentialing letter. For the EUS faculty or ED Director at the graduate’s new institution,
this letter provides a detailed description of the EUS training curriculum completed, including the number of
quality reviewed training exams completed by application and overall, and performance on SDOTs and
simulation assessments. Example letters and other EUS program and education resources can be found at
https://www.acep.org/emultrasound/resources/running-a-program/.
Practice-Based Pathway
For practicing EM attendings who completed residency without specific EUS training, a comprehensive
longitudinal curriculum, multi-day course, series of short courses, or preceptorship is recommended.
66
Shorter
courses covering single or a combination of applications may provide initial or supplementary training.
67
As
part of pre-course preparation, EUS faculty must consider the unique learning needs of the participating

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 8 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
trainees. The course curriculum should include trainee-appropriate learning objectives, educational methods
and assessment measures as outlined by these guidelines. If not completed previously, then introductory
training on US physics and knobology is required prior to training in individual applications. Pre-course and
post-course online learning may be utilized to reduce the course time spent on traditional didactics and
facilitate later review. Small group hands-on instruction with EUS faculty on models, simulators, and task
trainers provides experience in image acquisition, interpretation, and integration of EUS exam findings into
patient care. See Appendix 5.
Preceptorships typically lasting 1-2 weeks at an institution with an active EUS education program have also
been utilized successfully to train practicing physicians. Each preceptorship needs to begin with a discussion
of the trainees’ unique educational needs, hospital credentialing goals as well as financial support for faculty
teaching time. Then the practicing physician participates in an appropriately tailored curriculum typically in
parallel with ongoing student, resident, fellow and other educational programming.
Similar to an EM Resident EUS credentialing letter, course and preceptorship certificates should include a
description of the specific topics and applications reviewed, total number of training exams completed with
expert supervision, performance on other course assessment measures such as SDOTs or simulation cases, as
well as the number of CME hours earned. These certificates are then given to local EUS faculty or ED
directors to document training.
Physician Assistants, Nurse Practitioners, Nurses, Paramedics, and other EM clinicians
In many practice environments, EUS faculty often provide POCUS training and ongoing support to other
clinicians including Physician Assistants, Nurse Practitioners, Nurses, Paramedics, Military Medics and
Disaster Response Team members. Supervision should align with that defined by the ACEP policy statement,
Guidelines Regarding the Role of Physician Assistants and Nurse Practitioners in the Emergency
Department.
68
The recommendations in these ACEP guidelines should be utilized by EUS faculty when
providing such training programs. Pre-course preparation needs to include discussions with staff leadership
to define role-specific learning needs and applications to be utilized. Introductory US physics, knobology,
and relevant anatomy and pathophysiology are required prior to training in targeted applications.
Ongoing Education
As with all aspects of EM, ongoing education is required regardless of training pathway. The amount of
education needed depends on the number of applications being performed, frequency of utilization, the local
practice of the individual clinician, and developments within EUS and EM. Individual EUS credentialed
physicians should continue their education with a focus on EUS learning as a recurring component of
educational activities. Educational sessions that integrate EUS into daily practice are encouraged and do not
have to be didactic in nature, but instead may be hands-on or online. Recommended EUS educational
activities include EUS conference attendance, online educational activities, preceptorships, teaching,
research, hands-on training, program administration, quality assurance, image review, written examinations,
textbook and journal readings, as well as morbidity and mortality conferences inclusive of EUS cases. EUS
quality improvement is an example of an activity that may be used for the completion of the required ABEM
Improvement in Medical Practice Activity.
Fellowship Training
Fellowships provide the advanced training needed to create future leaders in evolving areas of medicine
such as EUS. This advanced training produces experts in EUS and is not required for the routine
utilization of EUS.

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 9 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
An Advanced Emergency Medicine Ultrasonography (AEMUS) fellowship provides a unique, focused, and
mentored opportunity to develop and apply a deeper comprehension of advanced principles, techniques,
applications, and interpretative findings. Knowledge and skills are continually reinforced as the fellow learns
to effectively educate new trainees in EUS, as well as clinicians in other specialties and practice environments.
A methodical review of landmark and current literature, as well as participation in ongoing research, creates
the ability to critically appraise and ultimately generate the evidence needed for continued improvements in
patient care through CUS. Furthermore, a fellowship provides practical experience in EUS program
management including quality assurance review, medical-legal documentation, image archiving,
reimbursement, equipment maintenance, and other administrative duties of an EUS program director or
System-Wide CUS Director.
69
Recommendations for fellowship content, site qualifications, criteria for fellowship directors, and minimum
graduation criteria for fellows have been published by national EUS leaders and within the ACEP Emergency
Ultrasound Fellowship Guidelines. Each fellowship program’s structure and curriculum will vary slightly
based on local institution and department resources. ABEM has helped to standardize AEMUS fellowships
through a fellowship program accreditation process involving EUFAC (Emergency Ultrasound Fellowship
Accreditation Council).
70
ACEP participates in this as a nominating organization to EUFAC. At all fellowship
programs, mentorship and networking are fundamental to a fellow’s and program’s ultimate success. Both
require significant EUS faculty time for regular individual instruction as well as participation in the clinical
US community locally and nationally. Accredited fellowships are required to supply sufficient US faculty
support to maintain the training environment. Hence, institution and department leadership support is
essential to ensuring an appropriate number of EUS faculty, each provided with adequate non-clinical time.
For the department, a fellowship speeds the development of an EUS program. Fellowships improve EM
resident training resulting in increased performance of EUS examinations. Furthermore, a fellowship training
program may have a significant positive impact on overall EUS utilization, timely QA review, faculty
credentialing, billing revenue, and compliance with documentation. For an institution, an EUS fellowship
provides a valuable resource for other specialties just beginning POCUS programs. Collaborating with EUS
faculty and fellows, clinicians from other departments are often able to more rapidly educate staff and create
effective POCUS programs.
Advanced Emergency Medicine Ultrasonography was approved as a Focused Practice Designation (FPD) by
the American Board of Medical Specialties in 2017. To be eligible for FPD certification in Advanced
Emergency Medicine Ultrasonography, EUS fellows must be board certified by ABEM in EM and complete
a EUS Fellowship that has been accredited by the new Emergency Ultrasound Fellowship Accreditation
Council. After graduating, qualified fellows are then eligible to take the Advanced Emergency Medicine
Ultrasonography Fellowship Examination now offered by ABEM to earn their FPD certification.
71,72
US in Undergraduate Medical Education
EM faculty often lead efforts to improve Undergraduate Medical Education (UME) through the early
integration of US. During the preclinical years, US has been demonstrated to be an effective educational
method to reinforce student understanding of anatomy, physical examination skills, pathology and bedside
diagnostic skills. During the clinical years, these students are able to utilize POCUS for clinical diagnosis on
specific rotations. US exposure in UME can provide a solid foundation for the integration of POCUS into
their clinical practice during Graduate Medical Education (GME).
Integrating US into UME
Integration of US into pre-clinical UME often begins with medical student and faculty interest.
73
By working

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 10 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
closely with a medical school’s curriculum committee, US may then be incorporated as an engaging hands-
on educational method to enhance learning within existing preclinical courses. Widespread POCUS
utilization by different specialties within a medical school’s teaching hospitals often helps to provide the
needed faculty time and expertise, teaching space, and US equipment. Ongoing annual education then requires
local departmental and medical school leadership support, as well as continued organized collaboration
between faculty from participating specialties.
Innovative educational methods again provide the opportunity for clinical US faculty to focus on small group
hands-on instruction as described in the innovative education section.
Many academic departments that
currently offer clinical rotations within EM already include an introduction to EUS as a workshop or a set
number of EUS shifts. Dedicated EUS elective rotations provide an additional opportunity for medical
students interested in EM and other specialties utilizing POCUS to participate in an EUS rotation adapted to
their level of training and unique career interests. See Appendix 6 for recommendations for POCUS medical
school rotations.
US in UME continuing into POCUS in GME
UME US experience should prepare new physicians to more rapidly utilize POCUS to improve patient care
during graduate medical education (GME) training. Medical students therefore should graduate with a basic
understanding of US physics, machine operation, and common exam protocols such as US guided vascular
access. Medical students matriculating from a school with a detailed integrated US curriculum across the pre
and clinical years, as well as those completing an elective POCUS rotation, should be provided with a
supporting letter describing didactics, hands-on training, and total examinations. Although all trainees need
to complete the EUS residency requirements, trainees with basic proficiency in US from UME training may
progress more rapidly and ultimately achieve higher levels of EUS expertise during GME. Additionally, these
residents may provide considerable EUS program support as peer-to-peer instructors, residency college
leaders, investigators and potentially future fellows.
Section 4 – Hospital Credentialing and Privileging
Implementing a transparent, high-quality, verifiable and efficient credentialing system is an integral
component of an EUS program. The medical staff at a hospital are governed by bylaws. Included within
these bylaws are credentialing and re-credentialing requirements and responsibilities, including the
delineation of privileges of clinicians. A high quality and verifiable credentialing process is a duty owed by
a hospital to its patients. The hospital can be deemed negligent in the event of a bad patient outcome if the
credentialing process is found to be deficient.
An EUS director, along with the department leadership, should develop policies and guidelines pertaining to
EUS. The department should follow the specialty-specific guidelines set forth within this document for their
credentialing and privileging process. Pertaining to clinician performed US, the American Medical
Association (AMA) House of Delegates in 1999 passed a resolution (AMA Res. 802, I-99) recommending
hospitals’ credentialing committees follow specialty-specific guidelines for hospital credentialing decisions
related to US use by clinicians.
74
This resolution became AMA policy, Privileging for Ultrasound Imaging,
74
and affirms that US imaging is within the scope of practice of appropriately trained physician specialists and
provides clear support for hospital credentialing committees to grant EUS privileging based on the specialty-
specific guidelines contained within this document without the need to seek approval from other departments.
Furthermore, HR 802 states that opposition that is clearly based on financial motivation meets criteria to file
an ethical complaint to the AMA.

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 11 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
The provision of clinical privileges in EM is governed by the rules and regulations of the department and
institution for which privileges are sought. The EM Chairperson or Medical Director or his/her designee (eg,
EUS director) is responsible for the assessment of CUS privileges of emergency physicians. When a physician
applies for appointment or reappointment to the medical staff and for clinical privileges, including renewal,
addition, or rescission of privileges, the reappraisal process must include assessment of current competence.
The EM leadership will, with the input of department members, determine how each emergency physician
will maintain competence and skills and the mechanism by which each physician is monitored.
EM departments should list EUS within their core EM privileges as a single separate privilege for
“Emergency US” or US applications can be bundled into an “US core” and added directly to the core
privileges. EM should take responsibility to designate which core applications it will use, and then track its
emergency physicians in each of those core applications. To help integrate physicians of different levels of
sonographic competency (graduating residents, practicing physicians, fellows and others), it is recommended
that the department create a credentialing system that gathers data on individual physicians, which is then
communicated in an organized fashion at predetermined thresholds with the institution-wide credentialing
committee. This system focuses supervision and approval at the department level where education, training,
and practice performance is centered prior to institutional final review. As new core applications are adopted,
they should be granted by an internal credentialing system within the department of emergency medicine.
Eligible clinicians to be considered for privileging in EUS include emergency physicians, physician
assistants, nurse practitioners, or other healthcare workers who complete the necessary training as specified
in this document via residency training or practice-based training (see Section 3 – Training and Proficiency).
After completing either pathway, these skills should be considered a core privilege with no requirement
except consistent utilization and ongoing education. At institutions that have not made EUS a core privilege,
submission of 5-10% of the initial requirement for any EUS application is sufficient to demonstrate continued
proficiency.
Sonographer certification or EUS certification by external entities is not an expected, obligatory or an
encouraged requirement for EUS credentialing.
75
Those physicians who specialize in AEMUS will have
acquired a greater breadth and depth of knowledge in advanced techniques, research, and quality
improvement skills. The FPD recognizes expertise held by emergency physicians with sophisticated,
comprehensive knowledge of advanced emergency ultrasonography and is available only to ABEM-certified
physicians.
Regarding re-credentialing or credentialing at a new health institution or system, ACEP recommends that
once initial training in residency or by practice pathway is completed, credentialing committees recognize
that training as a core privilege, and ask for proof of recent updates or at most a short period of supervision
prior to granting full privileges.
In addition to meeting the requirements for ongoing clinical practice set forth in this document, physicians
should also be assessed for competence through the CQI program at their institution. (See Section 6-Quality
and US Management) The Joint Commission (TJC) in 2008 implemented a new standard mandating detailed
evaluation of practitioners’ professional performance as part of the process of granting and maintaining
practice privileges within a healthcare organization.
76
This standard includes processes including the Ongoing
Professional Practice Evaluation (OPPE) and the Focused Professional Practice Evaluation (FPPE). Specific
to FPPE and US credentialing, for infrequently performed US examinations, FPPE monitoring can be
performed on a predetermined number of examinations (ie, review of the diagnoses made on the first 10 or
20 of a particular US examination). The FPPE process should: 1. Be clearly defined and documented with
specific criteria and a monitoring plan; 2. Be of fixed duration; and 3. Have predetermined measures or

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 12 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
conditions for acceptable performance. OPPE can incorporate EUS quality improvement processes. US
directors should follow these guidelines when setting up their credentialing and privileging processes.
Section 5 – Specialty Certification
ABEM instituted specialty certification using a focused practice designation (FPD) pathway in 2021. ABMS
created the FPD process to allow subspecialty recognition. Certification through the FPD process is available
only to ABEM diplomates who have advanced training or expertise in emergency ultrasound. Details on the
process and requirements are available at www.ABEM.org. The lack of achieving AEMUS FPD does not
imply a lack of skill in ultrasound and FPD should not be viewed as required for use of ultrasound by EM
graduates or as a requirement for billing for ultrasound.
Section 6 – Quality and US Management
To ensure quality, facilitate education, and satisfy credentialing pathways, a plan for an EUS quality
improvement (QI) process should be in place. This plan should be integrated into ED operations. The facets
of such a program are listed below. Programs should strive for meeting these criteria and may seek
accreditation through the Clinical Ultrasound Accreditation Program (CUAP).
Emergency US Director
The emergency US director is a board-eligible or -certified emergency physician who has been given
administrative oversight over the EUS program from the EM Chairperson, director or group. This may be a
single or group of physicians, depending on size, location(s), and coverage of the group. Specific
responsibilities of an US director and associates may include:
- Maintaining compliance with overall program goals: educational, clinical, financial, and academic.
- Selecting appropriate US machines, probes and equipment for the clinical care setting.
- Providing a maintenance care plan to ensure quality, cleanliness, disinfection and storage.
- Overseeing credentialing and privileging for physicians, physician assistants, nurse practitioners, and
other healthcare workers within the group and/or academic facility.
- Providing educational resources for physicians, physician assistants, nurse practitioners, and other
healthcare workers seeking credentialing, which may include in-house and/or outsourced educational
content.
- Monitoring and ensuring documentation of individual physician privileges, educational experiences, and
US scans performed.
- Developing, maintaining, and improving an adequate QA process in which physician scans are reviewed
for quality in a timely manner and from which feedback is generated.
The emergency US director must be credentialed as an emergency physician and maintain privileges for EUS
applications. If less than two years in the position of US director, it is recommended that the director have
either: 1) graduated from an EUS fellowship either EUFAC or non-EUFAC accredited, 2) participated in an
EUS management course, or 3) completed an EUS preceptorship or mini-fellowship. For ABEM-boarded
directors, obtaining and maintenance of the Focused Practice Designation in Advanced EM Ultrasonography
is strongly encouraged.
71
Supervision of US Training and Examinations
Ultrasound programs involved in training must have clearly written policies regarding educational US
examinations relevant to each type of learner. (See Sections 2, 3, and 4)
ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 13 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
US Documentation
Emergency US is different from consultative US in other specialties as the emergency physician not only
performs but also interprets the US examination. In a typical hospital ED practice, US findings are
immediately interpreted, and should be communicated to other physicians and services through reports in the
electronic medical record (EMR). Emergency US documentation reflects the nature of the exam, which is
focused, goal-directed, and performed at the bedside contemporaneously with clinical care. This
documentation may be preliminary and brief in a manner reflecting the presence or absence of the relevant
findings. Documentation, as dictated by regulatory and payor entities, may require more extensive reporting
including indication, technique, findings, and impression. US reports should be available in a timely manner
to allow review by members of the health care team and consultants.
77
During out-of-hospital, remote, disaster, and other scenarios, US findings may be communicated by other
methods within the setting constraints. Incidental findings should be communicated to the patient or follow-
up clinician. Discharge instructions should reflect any specific issues regarding US findings in the context of
the ED diagnosis. Hard copy (paper, film, video) or digital US images should be saved within the ED or
hospital archival systems. Digital archival with corresponding documentation is optimal and recommended.
78
Finally, documentation of emergency US procedures should result in appropriate reimbursement for services
provided.
9,79
(See Section 7 – Value and Reimbursement)
Quality Improvement Process
A QI process is an essential part of any US program and should include a QA component focused on review
of each clinician’s use of ultrasound. QA should evaluate use of ultrasound in indicated clinical scenarios,
technical competence for image acquisition and accurate interpretation. Technical parameters to be evaluated
might include image resolution, anatomic definition, and other image quality acquisition aspects such as gain,
depth, orientation, and focus. In addition, QA should compare the impression from the EUS interpretation to
patient outcome measures such as consultative US, other imaging modalities, surgical procedures, pathology
reports or patient clinical outcome.
The QI system design should strive to provide timely feedback to physicians. Any system design should have
a data storage component that enables data and image recall. A process for patient callback should be in place
and may be incorporated into the ED’s process for calling patients back. Callbacks should occur when the
initial image interpretation, upon QA review, may have been questionable or inappropriate and of clinical
significance. In all cases, the imaging physician is informed of the callback and appropriate
counseling/training is provided. All studies obtained by non-credentialed physicians should be reviewed.
Once clinicians are credentialed, programs should strive to sample a significant number of studies from each
clinician that ensures continued competency. Due to the varieties of practice settings the percentage of studies
undergoing review should be determined by the US director and should strive to protect patient safety and
maintain competency. While this number can vary, a goal of 5-10% may be reasonable, adjusted for the
experience of the clinician and novelty of the US application in that department.
The general data flow in the QA system is as follows:
1. Images obtained by the imaging clinician should be archived, ideally on a digital system. These
images may be still images or video clips and should be representative of the US findings.
2. Clinical indications and US interpretations should be documented.
3. These images and data are then reviewed by the US director or a designee.
4. Reviewers evaluate images for accuracy and technical quality and submit the reviews back to the
imaging clinician.

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 14 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
5. EUS studies are archived and available for future review should they be needed.
QA systems currently in place range from thermal images and logbooks to complete digital solutions. Finding
the system that works best for each institution will depend on multiple factors, such as machine type,
administrative and financial support, and physician compliance. Current digital management systems offer
significant advantages to QA workflow and archiving.
US QA may also contribute to the ED’s local and national QI processes. US QA activities may be included
in professional practice evaluation, practice performance, and other quality improvement activities. Measures
such as performance of a FAST exam in high acuity trauma, detection of pregnancy location, and use of US
for internal jugular vein central line cannulation are examples of logical elements in an overall quality plan.
In addition, US QA databases may contribute to a registry regarding patient care and clinical outcomes.
US Machines, Safety, and Maintenance
Dedicated US machines located in the ED for use at all times by emergency physicians are essential. Machines
should be chosen to handle the rigors of the multi-user, multi-location practice environment of the ED.
80
Other
issues that should be addressed regarding emergency US equipment include: regular in-service of personnel
using the equipment and appropriate transducer care, stocking and storage of supplies, adequate cleaning of
external and internal transducers with respect to infection control, maintenance of US machines by clinical
engineering or a designated maintenance team, and efficient communication of equipment issues. Clinicians
using ultrasound should follow common ED US safety practices including ALARA (as low as reasonably
achievable), probe decontamination, and machine maintenance. A policy should be in place to address the
use of non-dedicated US machines used by emergency medicine clinicians in the department, such as personal
handheld ultrasound devices.
81
Risk Management
US can be an excellent risk reduction tool through 1) increasing diagnostic certainty, 2) shortening time to
definitive therapy, and 3) decreasing complications from procedures. An important step to managing risk is
ensuring that physicians are properly trained and credentialed according to national guidelines such as those
set by ACEP and outlined in this document. Proper quality assurance and improvement programs should be
in place to identify and correct substandard practice. The greatest risk regarding EUS is lack of its use in
appropriate cases.
82
The standard of care for emergency US is the performance and interpretation of US by a credentialed
emergency physician within the limits of the clinical scenario. Physicians performing US imaging in other
specialties or in different settings have different goals, scopes of practice, and documentation requirements,
and consequently should not be compared to EUS. As EUS is a standard emergency medicine procedure, it
is included in any definition of the practice of emergency medicine with regards to insurance and risk
management.
Section 7 – Value and Reimbursement
Value in health care has been defined as outcomes that matter to patients relative to cost.
83
The value of CUS
is maximized when time spent by the clinician prevents costly imaging, invasive therapeutics, unnecessary
consultations and produces accessible real-time results for the patient and the health care system.
Clinical US contributes to patient health in several ways:
1. Improving patient safety by reducing medical errors during procedures

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 15 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
2. Increasing patient satisfaction
3. Improving departmental resource utilization
4. Eliminating costly or invasive procedures
5. Improved clinical decision making
Reimbursement for US derives from Current Procedural Terminology (CPT) codes and their respective
relative value units (RVUs). The reimbursements for US are calculated on work performed by entities within
the healthcare system, with some going to physicians and some going to hospital entities.
9
The current system
assumes a similar workflow for all US. The evolution of CUS has changed the workflow for many clinicians.
From a practical standpoint, reimbursement from the performance of CUS occurs through two primary
mechanisms. One is billing for services rendered using Centers for Medicare and Medicaid Services (CMS)
guidelines, or direct billing. This is the way that most specialties get reimbursed for performing and
interpreting ultrasound and the rules are the same regardless of the specialty. Billing for ultrasound involves
the use of CPT codes that define the type of ultrasound performed and ICD-10 codes to support the reason
for the ultrasound. Billing for the performance and interpretation of CUS involves following rules determined
by CMS, as well as any applicable hospital or third-party rules on performance and documentation of CUS.
The second way for reimbursement of CUS in the ED is within the CMS rules for general ED department
visits using the CMS chart leveling process. This is called evaluation and management (E&M) leveling.
Charts are coded as level 1 through level 5 with higher levels receiving greater reimbursement. Clinical
ultrasound use contributes to the chart leveling process by demonstrating increased complexity and medical
decision making by the treating clinician. A percentage of instances when a CUS is performed will result in
the visit being eligible for higher chart coding and subsequently higher reimbursement. Stated another way,
some patients imaged with ultrasound will have a higher chart level (and reimbursement) when compared to
an identical patient who did not receive a clinical ultrasound.
84,85
CMS Requirements such as documentation
detail and image retention for billing for clinical ultrasound performance and interpretation do not necessarily
apply for revenue obtained through E&M, but hospital or departmental policies would still apply.
The current workflow for CUS differs widely from the historical workflow in traditional imaging specialties.
While consultative US centers on providing a work product for the interpreting physician, CUS centers on
the patient. The clinician evaluating the patient utilizes US at the patient’s bedside to answer a focused
question or guide an invasive procedure. The bedside physician takes over tasks that are attributed to the
hospital’s practice expenses, such as bringing the unit to the bedside, obtaining US images, and archiving
images for the medical record. Figure 3 shows the workflow in the model of CUS.
In addition to workflow differences, CUS has generally lower expenses related to capital equipment, physical
plant and supplies. The US machine is a less expensive mobile unit located in the ED and moved to the
patient’s bedside. Some hospitals are turning to lower cost archiving alternatives to PACS, including US
management systems (also known as middleware or workflow solutions) or cloud-based software solutions
which can allow readily accessible digitally archived images.
CPT values physician work (ie, wRVU) required for common EUS at approximately 40% of the global RVU
(total professional plus total technical). Active CUS programs allow the hospital to bill technical fees which
support the cost of the machine, supplies, and archiving/quality assurance software.
Efficiencies gained by incorporating US imaging in the care of emergency medicine patients can produce an
overall cost savings to the healthcare system. Clinical ultrasound may provide significant benefits by reducing
the needs for hospitalization, improved diagnosis and improved outcomes. With these benefits, shared savings
should be attributed appropriately to the entity which affected the change.
ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 16 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
A more detailed calculation of work depends on the specific clinical system organization and division of
labor/resources. Future alternative payment structures such as value-based purchasing, bundled payments, or
accountable care organizations (ACOs) should appropriately factor the resources, efficiency and value of
CUS into the value and reimbursement of emergency medical care.
Section 8 - Clinical US Leadership in Healthcare Systems
Many specialties in addition to EM utilize CUS across diverse patient care settings. Consequently, there is a
need for direction, leadership, and administrative oversight for hospital systems and health systems to support,
oversee, and administer an US workflow and due process in an organized, coordinated, and consistent manner.
Emergency physicians have decades of experience developing, maintaining, and administering CUS
programs within the ED. Furthermore, they have a broad scope of practice and interact with essentially all
specialties. Thus, they are uniquely positioned to serve in the role of Systemwide Clinical US Director.
Specifically, hospital and healthcare systems should:
1) consider CUS separate from consultative imaging and
2) use these guidelines and associated guidelines to design institutional clinical US programs; and
3) strongly consider experienced emergency physician US leaders for system leadership roles in CUS.
There are many approaches to institutional oversight of multidisciplinary CUS programs including and not
limited to: 1) consensus from major utilizers; 2) formation of a governing body such as a CUS steering
committee; or 3) creation of the position of an institutional CUS director. This person should have a broad
understanding of all applications and integration of CUS. Specific items to consider which require leadership
and coordination include policy development, equipment purchase, training and education, competency
assessment and credentialing, quality assurance, and value/reimbursement.
As the field continues to grow, there will be an increasingly large number of requests for CUS equipment.
There may be advantages to standardizing or coordinating hardware and software when possible so that
clinicians may share equipment across departments. This standardization may allow purchasing and cost
saving advantages due to bulk purchase negotiations as well as benefits for training with regard to machine
familiarity. Standardization may have some negative effects due to vendor exclusivity limiting access to
certain advancement in technologies and feature availability only available on other US products.
In academic and community centers there will be a need for educating trainees of different disciplines,
specialties, and levels of experience. Ideally, education for each individual specialty should come from within
that specialty. In the situation where education is needed and there are no leaders within a specific specialty,
then the training may fall to the director or committee as described above. In these cases, the director should
work with the leadership within the specialty to meet the training needs of that department. “Train the trainer”
programs are encouraged to help build intradepartmental capabilities.
It is crucial to develop subject matter experts within the hospital to meet the ever-increasing administrative,
clinical, and educational needs. Once these leaders are established, it will be useful to have the committee
and director oversee and coordinate to make sure these pillars are consistent across specialties, and that
resources and work effort are shared and not duplicated.
Credentials for each specialty should follow national guidelines and be specialty specific.
72
However, if
national training guidelines for specialties do not exist, the director and/or committee should create general
credentialing guidelines based on the ACEP structure. These should be flexible enough to meet the needs of
that specialty for their relevant applications.
ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 17 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
Quality assurance and quality improvement should be organized and run within a department. There may not
be subject matter experts with the time, qualifications, and/or interest in providing this workflow requirement.
In these cases, the director and/or committee should work with that department/specialty to develop a plan to
meet this need. Institutions must provide appropriate resources to system-wide programs. A CUS program
can be organized and structured by following the steps outlined in the ACEP System-Wide Ultrasound
Director committee documents.
69,86
Section 9 - Future Issues
Recent technological advances and miniaturization of US devices have improved access and overall US
imaging. Wireless transducers, handheld systems and app-based imaging connected via smart device are all
becoming the reality of CUS.
87-91
These enhancements represent novel and exciting forms of US technology
that expand the availability of US to new clinical settings due to increased portability and relative
affordability. These new devices are currently being evaluated in a variety of clinical settings and more
diverse situations that had not previously been possible.
While the benefits of handheld US devices are undeniable, concerns regarding operator qualifications, device
security, cloud storage, data ownership, disinfection protocols, reimbursement, patient confidentiality, and
safety are all serious concerns which continue to persist.
92,93
Non-CUS organizations have raised many of
these as potential risks to patient care when not properly addressed.
94
Though there are barriers surrounding
handheld US device use, many of these can be overcome by adhering to policies and guidelines developed
by organizations such as ACEP to maintain quality and ensure patient safety.
81
Transducer technology will continue to evolve, including high-resolution transducers that optimize
sonographic windows, integrated probe/machine devices, and devices that use existing and new computer
connections. Continuous advancements will allow clinicians to utilize US technology increasingly and reduce
inherent limitations and obstacles to use. However, cost remains one of most prominent barriers for
widespread use of some of the newer and potentially helpful technologies, such as electronic volumetric
transducers which allow the acquisition of a large volume of data with no movement of parts within the probe.
Currently, there is considerable variation with US workflow and standards; however, the number of vendors
in this space has fortunately increased significantly with several hardware manufacturers developing their
own workflow and image archiving solutions. The few long-established software-only solutions have been
joined by new third-party workflow and archiving vendors, offering more options to CUS users than ever
before.
The automation and integration of machine learning into CUS is yet another developing arena. Artificial
intelligence (AI) has the potential to dramatically increase the impact of CUS on patient care by assisting
with both image acquisition and interpretation. Multiple companies have developed a variety of machine
learning algorithms ranging from detection of B-lines on lung US, determination of left ventricular ejection
fraction, and enhanced visualization for needle guidance during procedures. The near future holds promise
for expanded cardiac assessment capabilities based on additional machine learning algorithms as well as
abdominal and musculoskeletal applications. While the progress of AI assistance in CUS has been much
slower than initially anticipated, the sheer volume of small and large vendors endeavoring to develop
clinically impactful applications will result in a significant expansion of AI-based tools available to CUS
users. Many CUS-focused vendors have realized that AI applications must provide customer solutions from
start to finish and now incorporate image guidance to locate the target window of interest and then perform
an automated assessment of anatomy or function. In the mid and long term, it is anticipated that AI
applications will be able to perform rapid and accurate ultrasound assessments more efficiently than humans.
Such changes, if realized, will drive down the skill level required to perform ultrasound in a clinically
meaningful way. However, the expansion and increased sophistication of machine learning algorithms in

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 18 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
CUS will risk an erosion of skills required to perform ever more complex ultrasound examinations. Patient
performed automated ultrasound is on the FDA radar and applications have already been submitted by
vendors for clearance. Unsupervised scanning by patients, or consumer-based automated ultrasound may
follow.
The implementation of new technologies has played a consistent and central role throughout the history of
medical malpractice. Although the evidence is sparse for CUS resulting in increased malpractice claims and
some published articles suggest the opposite, we should expect an increase in claims with an increase in
utilization. One only has to look to our radiology and obstetrical colleagues to realize that ultrasound related
claims will occur with some regularity and anecdotal evidence of more recent malpractice case filings
indicates plaintiff attorneys are beginning to target emergency physicians (both for failing to use and for using
ultrasound) more than previously seen.
Despite the proliferation of technology, the use of CUS is growing more slowly in non-academic practice
settings. Most of the evidence published to date originated from academic settings and more attention needs
to be paid in community practice settings, which represent the majority of patients seen globally. To have a
meaningful and widespread impact on patient care, it is crucial to integrate CUS into clinical practice outside
of academic settings. Physicians in these settings may not even be aware of benefits of ultrasound technology
including increased patient safety, improved workflow, and patient throughput as well as the expansion of
the examinations available to patients presenting to the ED. Unfortunately, the current community practice
dominance by contract groups, which have little incentive to support expansion of emergency ultrasound use,
means change will likely continue to occur slowly in those settings.
Telesonography is a rapidly developing model which allows transfer of US images and video from remote
locations to obtain consultation and treatment recommendations.
95
Recent advances in US technology,
informatics, cloud computing, and 5G networks can allow remote experts to direct on-site, less-experienced
sonographers to obtain and interpret images that can impact patient care in real-time. An expert CUS mentor
could potentially guide distant untrained health care workers geographically dispersed over multiple locations
around the world. This paradigm may be utilized across all applications including procedural assistance. The
practice of remote telesonography has the potential to improve quality of care in underserved communities in
both domestic and global settings. This is still a growing area with unclear reimbursement policies for
emergency medicine physicians that needs further guidance from CMS.
Physician assistants, nurse practitioners, nurses, emergency medical service personnel and others recognize
the potential in their practice settings and desire to learn appropriate applications. Emergency physicians
should continue to collaborate with our colleagues at local, regional and national levels to help educate and
implement appropriate training and practice standards for the safety of our patients. in addition, leadership,
supervision, and collaboration with physicians in other specialties will continue to be critical to assure the
safe, effective use of CUS.
Importantly, ultrasound should not be conceptualized as an extension of the physical examination. While this
was initially seen as a method to deflect criticism and breakdown resistance by some clinical specialties, it is
now more commonly utilized to advocate against appropriate reimbursement for a focused diagnostic
ultrasound examination at the point-of-care. This approach has already shown evidence of undermining
reimbursement and is likely to continue to do so, resulting in many of our current applications being
unreimbursed in the future, resulting in limitations in program resources, program expansion, and patient
access to care. Emergency physicians should continue to reinforce that CUS is a diagnostic modality, separate
from and far above the capabilities of the physical examination and reimbursement is fully indicated.
Finally, quality programs such as the Clinical Ultrasound Accreditation Program
96
will provide leadership to
EDs who can meet the criteria in this document. As CUS moves forward, continued high quality research in
ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 19 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
the field needs to occur. Future methodological improvements focused on patient outcomes are crucial for the
advancement of CUS within medicine. Multi-center studies producing higher levels of evidence will allow
the continued growth of CUS in emergency care. The future, while undeniably bright, still requires much
effort on the part of us all.
Section 10 – Conclusion
ACEP endorses the following statements on the use of emergency, clinical, point-of-care US:
1. Emergency, clinical point-of-care ultrasound performed, interpreted, and integrated into clinical care by
emergency physicians is a fundamental skill in the practice of emergency medicine.
2. The scope of practice of emergency US can be classified into categories of resuscitation, diagnostic,
symptom or sign-based, procedural guidance, and monitoring/therapeutics in which a variety of
emergency US applications exists, including the core applications of Aorta, Bowel,
Cardiac/Hemodynamic Assessment, Deep Venous Thrombosis (DVT),trauma, Hepatobiliary,
Musculoskeletal (MSK), Ocular, Pregnancy, Procedural Guidance, Skin and soft-tissue, Testicular,
Thoracic/Airway, Trauma, Ultrasound-Guided Nerve Blocks, and Urinary Tract.
3. Training and proficiency requirements should include didactic, experiential and integrative components
as described within this document.
4. Emergency US training in EM residency programs should be fully integrated into the curriculum and
patient care experience.
5. Emergency US should be considered a core credential for emergency physicians undergoing privileging
in modern healthcare systems without need for external certification.
6. US QA and management require appropriate resources including physician direction, dedicated US
machines, digital US management systems, and resources for QA.
7. Healthcare clinical point-of-care ultrasound programs optimally led by emergency physicians should be
supported with resources for leadership, quality improvement, training, hardware and software
acquisition and maintenance.
8. Emergency US is an independent procedure that should be reimbursed and valued, independent of the
ED history, physical examination, and medical decision-making.
9. Emergency physicians with advanced US expertise should contribute leadership in clinical
ultrasonography at the departmental, institutional, system, national, and international level.
10. Evolving technological, educational, and practice advancements may provide new approaches,
efficiencies, and modalities in the care of the emergent patient.
ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 20 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
Table 1. Emergency Medicine Ultrasound Definitions
Advanced Emergency Medicine
Ultrasonography (AEMUS)
US by emergency physicians with advanced training. This term
is used by the American Board of Emergency Medicine Focused
Practice Designation.
Focused Practice Designation (FPD)
A pathway created by American Board of Medicine Specialties
to recognize advanced training. The pathway is specialty
specific and applies to advanced knowledge in an area. The
American Board of Emergency Medicine offers an FPD in
AEMUS.
Point-of-care Ultrasound (POCUS)
US performed by clinicians at the patient’s bedside that answers
a specific clinical question. There are many somewhat
synonymous terms for US performed by EM physicians at the
patient’s bedside.
Emergency Ultrasound
US performed and interpreted by the clinician as an emergency
procedure and directly integrated into the care of the patient.
There are many somewhat synonymous terms for US performed
by EM physicians at the patient’s bedside.
Educational Ultrasound
US performed on a patient, volunteer, or in simulation that is not
intended to provide information to further the clinical care of
that individual.
Consultative Ultrasound
US performed by non-EM specialists at the request of an EM
physician. This US is generally distinct from emergency
ultrasound in its scope (less narrow) and purpose (diagnostic
question that can wait for a consultant).
Resuscitative Ultrasound
US use directly related to cardiac resuscitation (ACLS), general
medical resuscitation (eg, sepsis), or resuscitation from
unknown causes.
Diagnostic Ultrasound
US use in a diagnostic imaging capacity. Some diagnostic US
are performed in series to monitor physiologic changes.
Sign- or Symptom-Based Ultrasound
US used in a clinical pathway based upon the patient’s
symptoms or signs (eg, shortness of breath)
Therapeutic Ultrasound
US use as part of therapy for patient care
Ultrasound-Guided Procedure
US to guide a procedure in real-time
Ultrasound-Assisted Procedure
US used to assist with a procedure that is not performed in real-
time (eg, pre-procedural identification)
Limited Ultrasound
US imaging of an organ or organ system that is not
comprehensive. This term is used to represent a level of US for
coding and billing. Limited US are sometimes confused for
incomplete US where a complete set of needed images are not
recorded or performed.
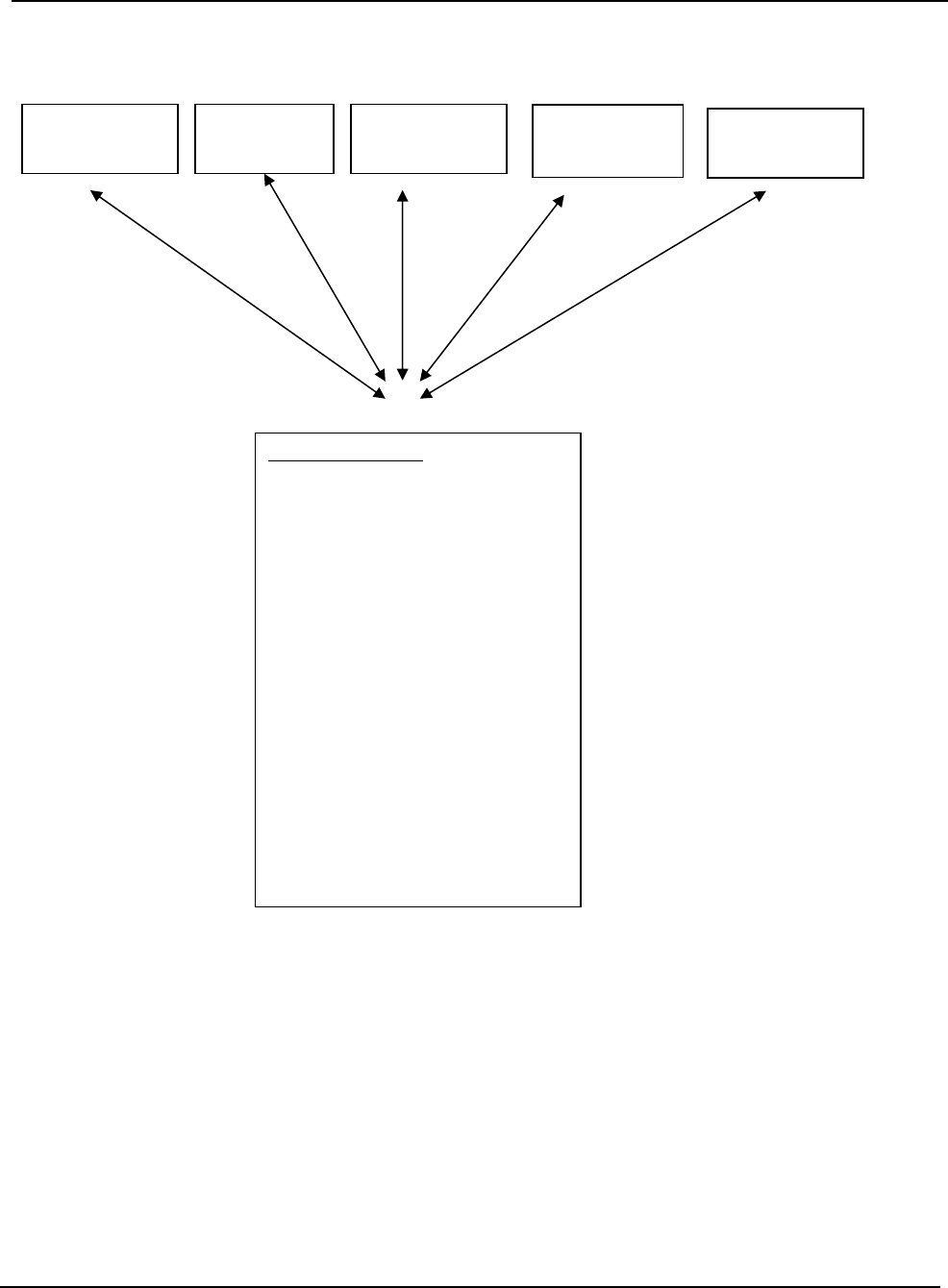
ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 21 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
Figure 1. ACEP 2023 Emergency US Guidelines Scope of Practice
Procedural
Guidance
Therapeutic
Resuscitative
Diagnostic
Symptom- or
Sign-Based
Core Applications
Aorta
Bowel
Cardiac/HD Assessment
Deep Vein Thrombosis (DVT)
Hepatobiliary
Musculoskeletal (MSK)
Ocular
Pregnancy
Procedural Guidance
Skin and Soft Tissue
Testicular
Thoracic/Airway
Trauma
Ultrasound-Guided Nerve Blocks
Urinary Tract
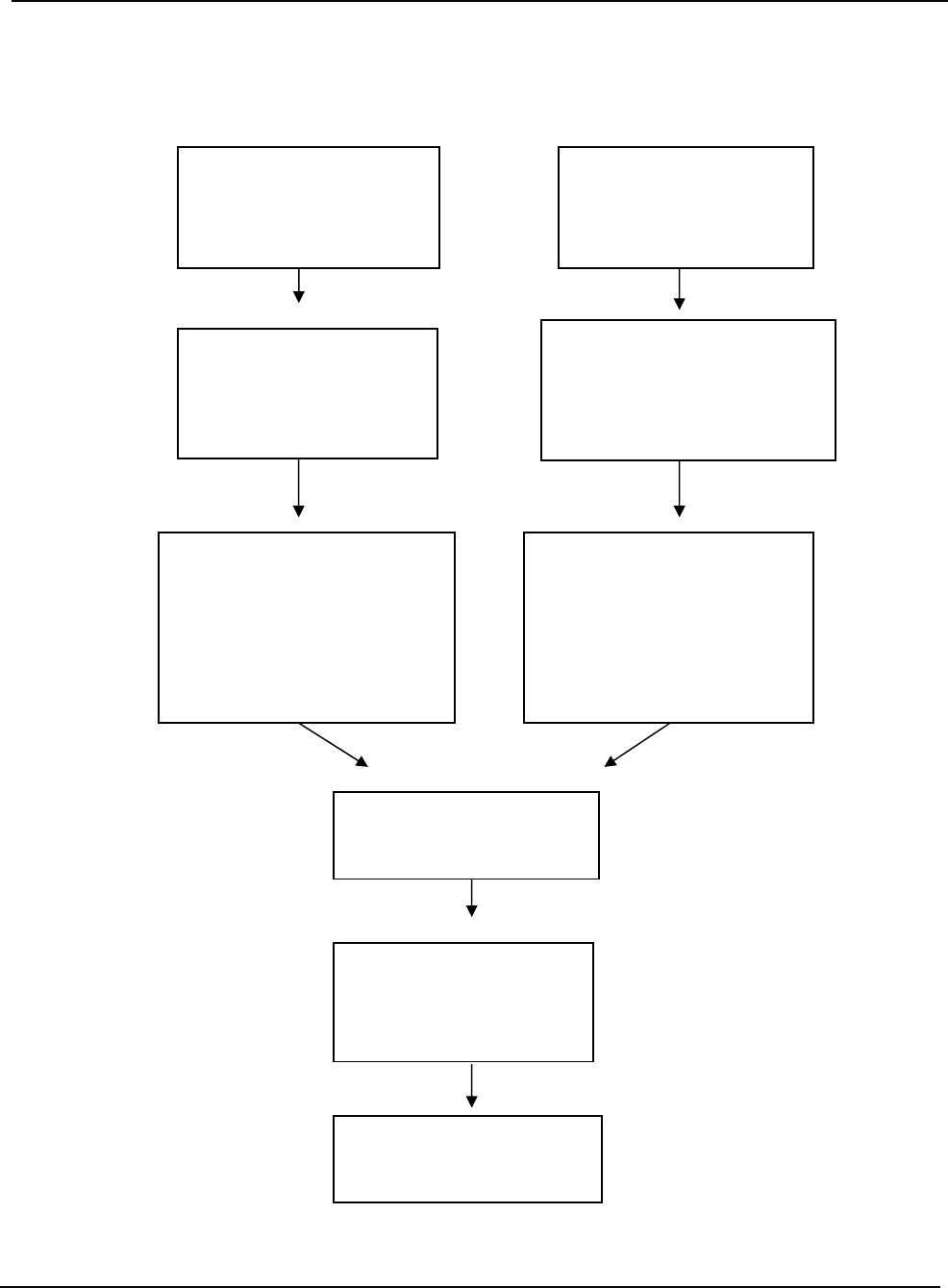
ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 22 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
Figure 2. Pathways for clinical ultrasound training, credentialing, and incorporation of new
applications
Residency Training Practicing Physician
Didactics
Experiential
Proficiency
Credentialing
Ongoing review and education
New Applications
Ultrasounds are obtained with
documentation and reviewed to
meet ACEP emergency
ultrasound proficiency
guidelines. Ultrasound available
for departmental and hospital
examination.
Residency Director and/or
Ultrasound Coordinator certifies
ultrasound training categorized by
the ACEP emergency ultrasound
proficiency guidelines and ABEM
“Model of the Clinical Practice of
Emergency Medicine”
Attends introductory
emergency ultrasound course
or courses that cover core
emergency US applications
Attends residency curriculum
covering emergency
ultrasound curriculum
New applications adopted
after CME, research, or other
training.
Performs ultrasounds under
supervision over-reads, gold
standards confirmatory testing or
patient outcome review within
departmental ultrasound plan
Training in residency per
Emergency Medicine
Residency Ultrasound
Guidelines and ACGME
Milestones
Acquired at local hospital
setting within departmental
privileges.
Quality review of ultrasound
performed continuously.
CME attended in accordance
with specialty guidelines.
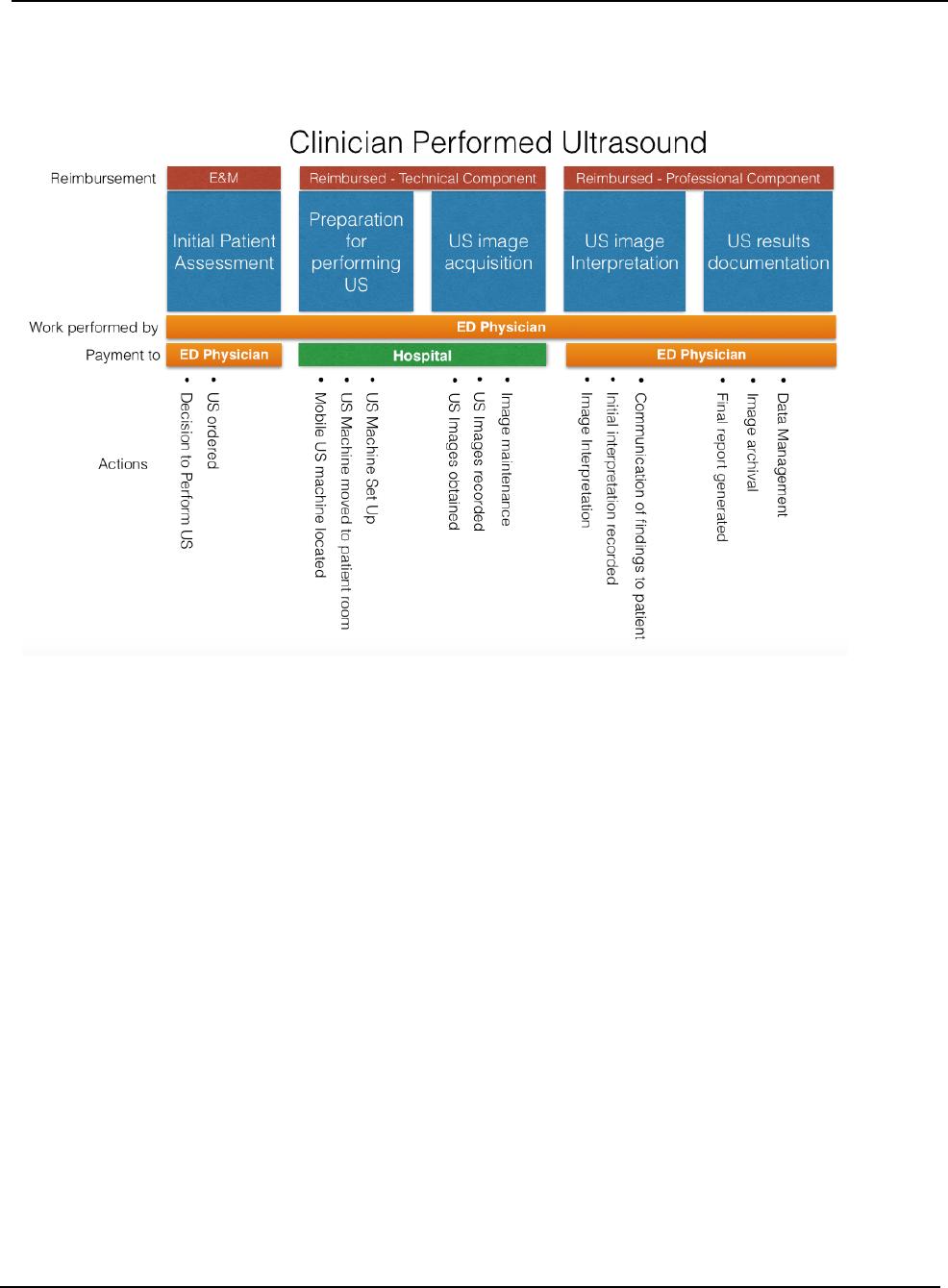
ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 23 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
Figure 3. Clinical Ultrasound Workflow

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 24 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
Appendix 1. Evidence for Core Emergency Ultrasound Applications
Aorta Ultrasound
Clinical ultrasound for aortic evaluation has been primarily focused to identify or exclude the presence or
absence of aortic aneurysms. A systematic review assessed the test characteristics of EP-performed US to
identify AAA against radiology performed US, MRI, CT, aortography, operative findings or autopsy reports
as criterion standards, with pooled data demonstrating sensitivity 97-100%, specificity 94-100%, positive
likelihood ratio of 10.8 to infinite, and negative likelihood ratio of 0-0.025 in detecting AAA
97
by EPs.
Another study evaluated student-performed ultrasound and was found to be superior to physical exams
performed by vascular surgery attendings in detecting AAAs,
98
thus US is a useful tool in detecting AAA,
even when performed by less experienced operators. The Screening for Abdominal Aortic Aneurysms Very
Efficiently (SAAVE) initiative by Medicare underscores the importance of AAA screening in certain
populations and has been shown to decrease AAA-related mortality and rupture,
99
but such screenings were
less successful in the busy emergency department setting.
100
While AAA is the most common aortic pathology seen on US, dissection and rupture are sometimes
encountered. In a prospective study, abdominal aortic dissection was identified on EP-performed ultrasound,
compared to CT angiography as the criterion standard, with sensitivity of 86%, specificity of 100%, and
negative predictive value 84%.
101
Typically rupture is difficult to discern on US, but some signs have been
proposed as highly specific for rupture, including irregularity of the aneurysmal shape, focal discontinuity of
the aortic wall, floating thrombus, interruption of the thrombus, para-aortic hypoechoic foci, as well as
concomitant peritoneal and/or retroperitoneal fluid.
102
When Type A aortic dissections are considered,
indirect signs such as, pericardial effusion, aortic regurgitation, and a dilated aortic root can also be identified
with bedside cardiac ultrasonography which may increase the sensitivity of this diagnosis.
103-105
However,
failure to identify these indirect signs cannot effectively rule out aortic dissection and may occasionally
warrant additional diagnostic modalities in the appropriate clinical scenario.
105
Bowel
Ultrasound has been studied extensively in the diagnosis of appendicitis for adults and children, with one
systematic review and meta-analysis demonstrating that POCUS has a sensitivity of 92% and a specificity of
96%.
2
Ultrasound is considered the first-line diagnostic study for appendicitis in children due to its lack of
ionizing radiation compared to CT and availability compared to MRI.
106
It has been demonstrated to decrease
CT scan utilization and shorten ED length of stay for children with suspected appendicitis.
107
Clinical ultrasound can also be utilized to assess for small bowel obstruction, diverticulitis, hernia, and
pneumoperitoneum. A large systematic review and meta-analysis found that US was 92.4% sensitive and
96.6% specific for diagnosing small bowel obstruction.
108
Among patients with suspected small bowel
obstruction, POCUS is more accurate than x-ray and one study found that US was 3 hours and 42 minutes
faster than CT.
109
Ultrasound has been demonstrated to be 92% sensitive and 90% specific for diverticulitis
with accuracy approaching that of CT.
110
A recent prospective observational study of emergency medicine
clinicians reported that US was 92% sensitive and 97% specific for diverticulitis,
111
while another study found
that integrating US into the clinical assessment reduced time to diagnosis by 3 hours and 53 minutes.
112
Ultrasound can identify pneumoperitoneum faster than CT and with greater accuracy than x-ray.
113
A 2018
systematic review and meta-analysis found that US was 91% sensitive and 96% specific.
114
Further, US can
provide information about abdominal wall masses and suspected hernias, with 97% sensitivity and 85%
specificity,
115
even guiding diagnosis and reduction of hernias at the bedside in real-time.
116

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 25 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
Among pediatric patients, evidence has been growing regarding the role of clinical ultrasound to identify
intussusception and hypertrophic pyloric stenosis. Intussusception is a common cause of pediatric bowel
obstruction and can be challenging to diagnose based on history and physical examination alone. Recent data
suggest POCUS for intussusception has comparable diagnostic accuracy to radiology-performed studies,
117
and a recent systematic review and meta-analysis reported a sensitivity of 94.9% and a specificity of 99.1%.
118
POCUS for intussusception can also improve time to reduction and shorten ED length-of-stay.
119
While data
on POCUS for hypertrophic pyloric stenosis are more limited, recent studies have reported high sensitivity
(96.6-100%) and specificity (94-100%),
120,121
as well as decreased length of stay.
121
Cardiac and Hemodynamic Assessment
Transthoracic focused cardiac US can be used to assess for pericardial effusion and tamponade, cardiac
activity for patients in cardiac or traumatic arrest, global assessment of left ventricular function, right heart
strain, and the detection of central venous volume status.
122
EP-performed cardiac US is highly sensitive and
specific for the diagnosis of pericardial effusion.
123
In patients with penetrating chest trauma the use of
focused cardiac US expedited diagnosis of pericardial fluid and tamponade and lead to expedited treatment.
124
In traumatic and cardiac arrest, US has prognostic value.
125-127
The likelihood of survival is zero after
traumatic arrest when either pericardial fluid or cardiac activity are not visualized in cardiac US.
125
In a
multicenter study on 793 patients in cardiac arrest, cardiac activity with US was associated with an increased
survival to hospital admission (OR 3.6, 2.2-5.9) and hospital discharge (OR 5.7, 1.5-21.9). Although cardiac
standstill was associated with mortality, 0.6% patients survived to discharge.
127
Cardiac US has been incorporated into the management of hypotensive and dyspneic patients. In patients with
undifferentiated hypotension, EP-performed cardiac US assessment of left ventricular ejection fraction
correlates well with measurements obtained by cardiology,
128
and its use leads to improved diagnostic
accuracy for the etiology of hypotension.
129,130
IVC assessment correlates to central venous pressure and can
be useful in differentiating different shock states.
131,132
In patients with undifferentiated dyspnea, cardiac US
in combination with lung US can differentiate acute heart failure from other etiologies of shortness of breath
and guide acute management.
133,134
Based on a systematic review and meta-analysis of 31 studies, US was
the single most useful test for diagnosing acute heart failure.
134
Findings of right heart strain on EP-performed
cardiac US correlates well with cardiology interpretation.
135
In patients with pulmonary embolism, cardiac
US used for the detection of right heart strain is specific and can be used to risk stratify patients.
136-138
Deep Vein Thrombosis
Over the past 21 years several studies including systematic reviews and meta-analysis have been performed
regarding emergency physician performed limited venous compression sonography for the evaluation of
DVT. The overall congruity on the limited compression ultrasound in the evaluation of DVT consistently
demonstrated a pooled sensitivity between 90–95% and specificity between 91–98%.
139-141
In 2018, a multidisciplinary panel of experts convened at the Society of Radiologists Ultrasound Consensus
Conference to provide recommendations for the most appropriate point-of-care study for the diagnosis of
DVT ultrasound.
142
The consensus from the conference deemed the extended compression ultrasound (ECUS)
also referred to as the 3-point compression ultrasound to be the most appropriate point-of-care examination
for the diagnosis of DVT.
142,143
The ECUS has also been compared to the 2-point compression ultrasound (2-
CUS) which does not include evaluation of the isolated femoral vein. Despite the recommendations from
conference, a meta-analysis performed by Lee et al. demonstrated that 2-point and 3-point POCUS were both
excellent methods for the diagnosis of DVT with similar sensitivity and specificity in various settings with a
multitude of performers.
141
The pitfall to the 2-CUS, however, has been reported to miss 5% to 7% of isolated
femoral vein thrombosis.
144-146

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 26 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
The advantages for using POCUS in the evaluation of DVT is that it can be performed immediately at the
bedside with a device that is readily available. This has been demonstrated to provide a faster disposition for
patients undergoing POCUS for DVT assessment when compared with radiology department DVT
assessment (95 vs. 225 minutes).
147
Hepatobiliary System
The use of emergency US for hepatobiliary disease has centered on biliary inflammation and biliary
obstruction. With the combination of portability, lack of ionizing radiation, and acceptable test characteristics,
US is considered the preferred initial imaging modality for patients suspected of having acute cholecystitis.
148
POCUS by emergency physicians facilitates ED patient throughput: A retrospective review of 1252 cases of
suspected cholecystitis demonstrated that bedside emergency physician US vs radiology US evaluation
decreased length of stay by 7% (22 minutes) overall, and up to 15% (52 minutes) when patients were
evaluated during evening or nighttime hours.
149
POCUS for the diagnosis of acute cholecystitis is operator dependent and the reported sensitivities and
specificities in the literature vary widely. Although many sonographic criteria for acute cholecystitis exist
(including gallstones, thickened gallbladder wall, pericholecystic fluid, sonographic Murphy’s sign, and
common bile duct dilatation), gallstones are present in 95-99% of acute cholecystitis cases.
150
The finding of
gallstones is quite accessible to the EP using bedside US, and may be placed into the context of an individual
patient’s clinical presentation to determine if acute cholecystitis if present. The test characteristics for
gallstone detection by bedside US are: sensitivity 90-96%, specificity 88-96%, positive predictive value 88-
99% and negative predictive value 73-96%.
151-154
In patients without risk factors for acalculous cholecystitis,
one study reported the absence of gallstones on POCUS exam performed by emergency physicians effectively
rule-out acute cholecystitis, with excellent negative predictive value (100%).
150
A more recent prospective
validation study of the Bedside Sonographic Acute Cholecystitis Score (SAC),incorporating patient
symptoms as well as physical and sonographic exam findings by emergency physicians with diverse levels
of training, reported 100% sensitivity in ruling out acute cholecystitis when the SAC score was <2 and 95.7%
when >7.
155
The measurement and interpretation of common bile duct dilatation (CBD) to assess for complicated
obstructive biliary pathology is considered more technically challenging than simply determining the
presence or absence of gallstones. However, one prospective observational study showed that after a focused
hepatobiliary training, novice emergency medicine residents attained a moderate level of agreement (Cohen
Kappa = 0.79) with expert radiologists in detecting abnormal CBD dilation >6 mm, but only weak agreement
in regard to the overall measurements themselves (Cohen’s Kappa = 0.45).
156
Additionally, another
prospective emergency medicine study demonstrated the sensitivity and specificity of CBD dilation for
complicated biliary pathology (CBP) to be only 23.7% and 77.9%, respectively, while none of the 39 patients
with CBP had isolated CBD dilation with normal lab values.
157
When the diagnosis of complicated
gangrenous cholecystitis is considered, defects of wall enhancement on contrast enhanced ultrasound has
been reported to have a sensitivity between 85-91% and a specificity of 67.5-84.8% cholecystitis.
158
Musculoskeletal Ultrasound
Clinical ultrasonography is useful for an array of musculoskeletal applications. Clinical ultrasound can be
utilized to identify shoulder dislocations and reductions with one recent systematic review and meta-analysis
reporting 100% sensitivity and 100% specificity.
3
This same meta-analysis found that POCUS was 96.8%
sensitive and 99.7% specific for diagnosing associated fractures.
3
Another study found that POCUS reduced
time-to-diagnosis by 43 minutes, while only requiring 19 seconds to perform.
159
Ultrasound can also diagnose
joint effusions and guide needle insertion for arthrocentesis or injection.
160
One systematic review and meta-

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 27 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
analysis of knee arthrocentesis found that POCUS increased accuracy (risk ratio 1.21), increased aspiration
volume (weighted mean difference [WMD] 17 mL), and had less procedural pain (WMD -2.24/10) with no
difference in procedural duration.
161
Another study of emergency medicine residents randomized to
ultrasound-guidance versus landmark technique for aspiration of the hip, ankle, and wrist in a cadaver model
found that ultrasound guidance had higher success rates (96% vs 89%) and fewer aspiration attempts (median
1 vs 2).
162
For long bone fractures, one systematic review reported that POCUS had 64.7% to 100% sensitivity
and 79.2% to 100% specificity in adults.
163
In pediatric patients, POCUS is 93.1% sensitive and 92.9%
specific for long bone fractures.
163
If a fracture is present, ultrasound can also be utilized to guide the
hematoma block.
164
Clinical ultrasonography is also valuable for identifying muscle injuries, such as ruptures and tears.
165-168
One
study found that ultrasound had similar accuracy to MRI for diagnosing muscular tears.
169
Ultrasound can
also be used to diagnose infectious causes of muscle pathology such as myositis and pyomyositis.
170,171
In a
retrospective review of 65 cases of surgically-proven pyomyositis, sonographic results were consistent with
operative findings in 95% of cases.
172
Clinical ultrasound can be a valuable tool for tendon injuries, as well.
In a prospective, multicenter study by Wu et al. Emergency medicine physicians were able to diagnose
extremity tendon injuries using POCUS with 100% sensitivity and 95% specificity.
173
There is growing
evidence regarding the role of ultrasound for diagnosing tenosynovitis, with one study reporting that
ultrasound was 94% sensitive and 65% specific.
174,175
Ocular
Ocular ultrasound can be a valuable tool for assessing the posterior segment of the eye, as well as the lens,
pupils, and as a surrogate for increased intracranial pressure (ICP). Within the posterior segment, one meta-
analysis found that POCUS was 94.2% sensitive and 96.3% specific for retinal detachment.
176
Another large
multicenter trial of emergency medicine clinicians reported 96.9% sensitivity and 88.1% specificity for retinal
detachment.
177
That study also reported 81.9% sensitivity and 82.3% specificity for vitreous hemorrhage, as
well as 42.5% sensitivity and 96.0% specificity for vitreous detachment.
177
Another recent meta-analysis
found that POCUS was 100% sensitive and 97% specific for lens dislocation, and 100% sensitive and 99%
specific for intraocular foreign body.
178
Beyond the posterior segment, ocular ultrasound may also be beneficial in the evaluation of patients with
eyelid edema or trauma that would otherwise limit inspection of the orbit. Studies have demonstrated the role
of ocular ultrasound for the examination of extraocular movement and pupillary assessment.
179
Ultrasound
can also be utilized as a non-invasive surrogate for ICP assessment via measurement of the optic nerve sheath
diameter (ONSD) with a recent systematic review finding ONSD was 90% sensitive and 85% specific when
compared to direct ICP monitoring.
180
Furthermore, ultrasound is 82% sensitive and 76% specific for the
detection of optic disc elevation or papilledema which may assist in the identification of long standing
elevated ICP seen in patients with idiopathic intracranial hypertension.
181
Pregnancy
Emergency ultrasound is used to evaluate the symptomatic pregnant patient and is particularly valuable in the
symptomatic first trimester pregnant patient as it is able to provide a definitive diagnosis in 80% of cases.
182
The most common ultrasonographic findings in the first trimester include an indeterminate location of
pregnancy, an intrauterine pregnancy, ectopic pregnancy, molar pregnancy, or fetal demise. An ectopic
pregnancy is suggested if the endomyometrial mantle (EMM) thickness is less than 8mm, regardless of the
Beta-hCG value.
183,184
Identification of ectopic pregnancy in the ED has been shown to expedite care and
decrease the time to surgery.
185
In addition, visualization of free fluid in Morison’s pouch in patients with
suspected ectopic pregnancy can predict the need for operative intervention.
186

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 28 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
Identification of an intrauterine pregnancy by emergency ultrasound is a powerful rule out test for ectopic
pregnancy as supported by evidence from a systematic review and meta-analysis of 2,057 patients which
found that emergency ultrasound had a sensitivity of 99.3%, NPV 99.96%, and negative likelihood ratio of
0.08 for ruling out ectopic pregnancy.
187
Emergency ultrasound has also been shown to have high accuracy
for dating in the first trimester when compared to radiology ultrasound.
188
In addition, symptomatic first
trimester pregnant patients who received a focused emergency ultrasound compared to comprehensive
ultrasound had significantly decreased length of stay.
189
In the second and third trimester, emergency
ultrasound can be used to evaluate for signs of uterine rupture.
190-192
In the postpartum period, emergency
ultrasound can be used to diagnose retained placenta and help to expedite expert consultation and definitive
care.
193
Procedural Guidance
Ultrasound guidance has been utilized for a wide array of common ED procedures.
Ultrasound has been
demonstrated to improve success rates and reduce complications for internal jugular, subclavian, and femoral
central venous access,
194-196
with the Agency for Healthcare Research and Quality (AHRQ) reporting this as
one of the top 11 strategies to increase patient safety in the United States. Similar benefits have been seen
with arterial line placement, where US has been shown to increase first-attempt success rates (relative risk
[RR] 1.31), reduce number attempts to success (mean difference [MD] -1.26), shorten mean time to success
(MD -43.158 seconds), and lower complication rates (RR 0.39).
5
A 2021 meta-analysis comparing US-guided
PIV with the landmark-based approach reported that US was associated with greater likelihood of successful
cannulation (odds ratio [OR] 2.1), fewer attempts (standardized MD -0.272), and improved patient
satisfaction (standardized MD 1.467/10) with no difference in procedural length.
4
Beyond vascular access, US can be a valuable adjunct for lumbar puncture (LP) with one recent meta-analysis
reporting increased overall success (OR 2.22), fewer traumatic LPs (risk difference -16.4%), shorter time to
successful LP (adjusted MD -1.80 minutes), fewer mean needle passes (adjusted MD -0.61), and reduced
patient pain scores (adjusted MD -2.53/10) in the US group.
6
The data supporting ultrasound-guided abdominal paracentesis is less robust; however, ultrasound has been
shown to improve procedural success and decrease complications. Ultrasound is superior to physical exam
for determining the presence of ascites pre-procedurall,
197
and using ultrasound-guidance for paracentesis
leads to improved success rates compared with the landmark-based approach (95% vs 61%), decreased
bleeding complications (OR 0.32) and decreased hospital costs (MD -$6,262).
198,199
Similarly, ultrasound-
guidance for thoracentesis has been demonstrated to reduce complications, with one meta-analysis reporting
decreased pneumothorax rates when US was used (OR 0.3).
200,201
One randomized control trial evaluated the
use of US in the diagnosis and management of peritonsillar abscess.
202
Patients in the US cohort were
successfully aspirated more frequently (LR 2.0), had fewer consults (absolute difference -43%), and more
accurate diagnosis (LR 2.8). Finally, ultrasound-guided pericardiocentesis has become the standard within
cardiology (rather than a blind technique) based on several large observational trials which demonstrated a
high success rate (97-98%) and a low complication rate (4.7-7%).
203,204
Though emergency medicine specific
studies are lacking, this supports the role for ultrasound-guidance of pericardiocentesis.
Skin and Soft Tissue Ultrasound
Point-of-care ultrasound is a valuable tool for the diagnosis and management of skin and soft tissue abscesses.
A recent systematic review and meta-analysis found that POCUS was 94.6% sensitive and 85.4% specific for
differentiating abscess from cellulitis.
205
Among those with a high pretest probability, POCUS is 93.5%
sensitive and 89.1% specific.
205
Among those cases that are clinically unclear, POCUS is significantly more
accurate (91.9% sensitivity, 76.9% specificity) compared with physical examination alone (77.6% sensitivity,

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 29 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
61.3% specificity).
205,206
Moreover, the addition of POCUS led to a change in management in 10.3% of cases
with a number-needed-to-treat of 10.
205
Once an abscess is suspected, POCUS can identify nearby vasculature
and help differentiate it from a pseudoaneurysm using color Doppler.
207
POCUS can also help identify the
depth and margins of the abscess to guide the placement of the incision and assess for adequate drainage.
207
POCUS can also be used for the diagnosis and management of skin and soft tissue foreign bodies. It can
detect non-radiopaque foreign bodies that could be missed on standard radiographs with one systematic
review reporting that POCUS was 72% sensitive and 92% specific for foreign bodies.
208
It can also be used
for real-time guidance of foreign body removal and can assist in detecting surrounding structures.
Finally, clinical ultrasound can help diagnose more dangerous conditions such as necrotizing fasciitis (NF).
Although the concern for NF is typically a clinical diagnosis, POCUS can assist in earlier diagnosis, especially
in patients who are too unstable for other imaging modalities (eg, CT, MRI). One study found that POCUS
was 100% sensitive and 98.2% specific,
209
while another study reported a sensitivity of 88.2% and specificity
of 93.3% for the diagnosis of NF.
210
In resource-limited settings without CT or MRI, clinical ultrasound can
assist clinicians along with clinical gestalt in the diagnosis of NF. It is also easily repeatable and can be used
to evaluate for progression of NF at the bedside.
Testicular Ultrasound
Ultrasound is the first line diagnostic study in addition to the clinical history and physical exam in the
evaluation of the acute scrotum in the ED.
211
Emergent and urgent pathologic etiologies identified via
ultrasound include testicular torsion, torsion of the testicular or epididymal appendage, infections of the
scrotum, epididymis, and testis, strangulated herniation of abdominal contents into the scrotum, as well as
traumatic injuries of the testicle.
211
A recent review recommends grayscale and color Doppler to remain the
mainstays of acute scrotal evaluation, while contrast enhanced ultrasound and elastography are new
techniques that can improve sensitivity in equivocal cases.
212
Ultrasound has been found to be highly accurate in the diagnosis of pathology in the patient presenting with
acute scrotum in both the adult and pediatric populations.
213,214
Accuracy for adult EPs in evaluation of the
acute scrotum have been found to be highly sensitive (95%) and specific (94%) when compared with
radiology ultrasound.
215,216
Accuracy for pediatric EPs in evaluation of the acute scrotum have also been found
to be highly sensitive, with 100% sensitivity and 99.1% specificity in the diagnosis of testicular torsion.
217
A
recent systematic review and meta-analysis indicates that the “whirlpool” sign is pathognomonic in adult
patients suspected of having testicular torsion, but less useful in neonatal populations.
218
Clinical ultrasound
may be especially useful in patients suspected of Fournier’s gangrene as it has comparable sensitivity with
computed tomography and can be performed at the bedside for unstable patients.
219
A review of cases shows
that testicular ultrasound is also highly sensitive and specific (100% and 93.% respectively) in the diagnosis
of testicular rupture in the testicular trauma.
220
Thoracic/Airway
Considerable evidence supports the use of clinical ultrasonography to diagnose a variety of thoracic
conditions such as pulmonary edema, pneumonia, pulmonary contusion, and pleural effusion. These
conditions can be assessed dynamically over time in response to therapeutic interventions such as diuresis,
non-invasive ventilation, and antibiotics. POCUS assessment for B-lines is 83-92% sensitive and 84-92%
specific for pulmonary edema and congestive heart failure.
1,221
POCUS is 85-92% sensitive and 93% specific
for diagnosing pneumonia,
222,223
including 83-96% sensitivity and 84-93% specificity in children.
224,225
Amidst the global pandemic, thoracic POCUS has demonstrated 91% sensitivity and 63% specificity for
COVID-19 in the emergency department.
226
Additionally, POCUS evaluation for a focal B-pattern in patients

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 30 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
with thoracic trauma is 92% sensitive and 89% specific for pulmonary contusion.
227
Lastly, POCUS is 91%
sensitive and 92% specific for the diagnosis of pleural effusion.
228
For patients with undifferentiated dyspnea,
early performance of POCUS can decrease time to diagnosis and disposition.
229
Ultrasonography has also been increasingly recognized as a valuable tool for airway assessment and
management.
230
Prior to endotracheal intubation, POCUS can be utilized to predict difficulty of intubation,
with one study reporting that POCUS outperformed several common clinical decision tools.
231
After an
intubation has been performed, one large meta-analysis found that transtracheal ultrasound identified
endotracheal versus esophageal intubation with 99% sensitivity and 97% specificity.
232
This accuracy has
remained consistent regardless of transducer, technique, or endotracheal tube size.
233, 239
Lung sliding can be
used as an alternate tool to assess for endotracheal tube location, as well as for endobronchial intubation.
238,239
This has been supported by the American Heart Association guidelines for Advanced Cardiac Life Support,
which delineate clinical ultrasonography as a reasonable tool for confirming endotracheal intubation.
240
Finally, ultrasound can be utilized to identify the cricothyroid membrane in advance of a difficult intubation
and even guide cricothyroidotomy in patients requiring a surgical airway.
241,243
Trauma
The use of US in trauma patients to detect
intra-abdominal, intrathoracic, or pericardial hemorrhage has been
incorporated in most trauma center protocols and is a part of the ATLS guidelines.
244
A review of 11
prospective studies shows that the focused assessment with sonography in trauma (FAST) examination has
sensitivities ranging from 87-98% and specificities 99% -100% in detecting intraperitoneal fluid in patients
who suffer from blunt trauma.
245
The evaluation of the thorax for injury with ultrasound defines the extended
focused assessment with sonography in trauma (EFAST) examination. The scope of the EFAST includes the
detection of pneumothorax, intrathoracic hemorrhage, and/or pulmonary contusions.
246,247
Ultrasound is more
sensitive than chest radiograph in detecting a pneumothorax with lung point being a very specific sign,
however, delaying management to identify the lung point is not recommended.
248
The EFAST examination can be used to evaluate penetrating trauma for thoracic and cardiac injuries with
high sensitivities for detecting pathology that require acute intervention. A retrospective review of patients
with penetrating thoracic trauma demonstrated 100% sensitivity for the detection of pericardial effusion
which expedited diagnosis and management.
124
Alternatively, the evaluation for penetrating abdominal
trauma may vary by case but evidence demonstrates a low sensitivity therefore making it a limited screening
tool.
249
The use of the EFAST examination in trauma has improved patient care and resource utilization by decreasing
the time to operative management, decreasing patient’s exposure to ionizing radiation, shortening their length
of stay in the hospital, and lowering patient costs.
250, 251
Ultrasound Guided Nerve Blocks
Ultrasound-guided peripheral nerve blocks are an important part of a multi-modal approach to pain
management in the ED.
252
Nerve block indications have continued to expand, and studies have demonstrated
the benefits of EP performed nerve blocks including improved pain control, decreased opioid use, and
decreased length of stay, to name a few. Overall safety for nerve blocks is also high, with data suggesting the
risk of peripheral nerve injury being as low as 0.03% and local anesthetic systemic toxicity occurring in 1.3
per 10,000 patients.
253,254
The most commonly performed nerve blocks include brachial plexus blocks, truncal
blocks, hip blocks and extremity blocks.

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 31 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
Brachial plexus blocks, including the superficial cervical plexus, RAPTIR, interscalene and supraclavicular
brachial plexus block, have been used for shoulder dislocation reductions, proximal humerus fractures, elbow,
wrist and hand lacerations and fractures. One randomized study demonstrated shorter length of stay using the
interscalene brachial plexus block for shoulder dislocation reduction compared to moderate sedation.
255
Truncal blocks, including the serratus anterior plane block (SAPB), erector spinae plane block (ESP) and
transversus abdominis plane block have been used for rib fractures, thoracostomy tube placement, herpes
zoster, renal colic, pancreatitis, lumbar transverse process fractures, and mechanical back pain.
256
One RCT
showed significant reduction in pain scores up to 24 hours after the block in patients who received a SAPB
block compared to a control group receiving tramadol.
257
Studies have found that patients who received ESP
for rib fractures had a significant reduction in pain scores
258
and improvement in inspiratory capacity.
256
Another randomized study found that patients with renal colic who received an ESP block compared to those
who received an NSAID had significantly better pain control, lower rates of opioid consumption and greater
patient satisfaction.
259
Transversus abdominis plane blocks have been used for pain control from post-op
hernias, abdominal wall abscesses, and appendicitis.
260,261
Nerve blocks such as the fascia iliaca, femoral nerve, and pericapsular nerve group block (PENG) are used
for pain control for hip fractures. These blocks are an important component of multimodal analgesia that is
recommended by the American Academy of Orthopaedic Surgeons
262
and recognized as best practice by the
American College of Surgeons.
263
Systematic reviews of multiple randomized controlled studies have found
that patients who received a nerve block for hip fracture had reduced pain on movement, decreased rates of
delirium and chest infection, and decreased time to mobilization.
264
When performed in the ED, fascia iliaca
blocks have been shown to decrease opioid consumption, length of stay, and hospital admission within 30
days of hip fracture.
265,266
In addition, the PENG block has been successfully used to control pain from non-
operative pelvic fractures.
267
Upper extremity forearm blocks and lower extremity blocks such as the popliteal sciatic, tibial, transgluteal
sciatic, sural, and adductor canal blocks have been performed for extremity injuries including fractures, burns,
abscesses, dislocation reductions, lacerations, and radicular leg pain.
268,269
One small randomized study found
that patients with hand injuries randomized to receive forearm nerve blocks had significant reduction in pain
compared to the control group who received usual care.
270
Urinary Tract
The use of EUS in the urinary tract has primarily been used for detection of hydronephrosis and bladder status
but has also been used to evaluate for renal masses, cystic structures, and foley catheter placement. A
multispecialty panel with representation from EM, urology, and radiology recommends US evaluation of the
patient with suspected renal colic in conjunction with urinalysis in almost all clinical scenarios except for the
extreme elderly.
271
Bedside renal US can decrease ED length of stay without increasing patient bounce backs
in patients suspected of having renal colic.
272
A large systematic review and meta-analysis of clinical renal
US showed a pooled sensitivity of 70.2% and specificity of 75.4%
271,273
for the evaluation of renal colic.
When only moderate or severe hydronephrosis were considered, the specificity increased to 94.4%.
271
Accuracy of bedside US by fellowship trained EP is comparable to that of radiology US and CT imaging for
imaging patients with suspected renal colic.
274,275
Furthermore, ultrasound evaluation of the patient with renal
colic has not shown to miss clinically significant alternate diagnoses in the majority of patients.
271,274,276
Evidence on evaluation of the bladder primarily focuses on volumetric measurements in the clinical setting.
Volumetric measurements of the bladder have been useful especially in pediatric populations where it has
shown to improve first pass success of catheterization.
277

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 32 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
Appendix 2. Evidence for Advanced Emergency Ultrasound Applications
Adnexal Pathology
The use of CUS to evaluate pelvic pain in the non-pregnant female may facilitate the diagnosis of adnexal
pathology such as ovarian torsion, tubo-ovarian abscess (TOA), and ovarian cysts. The evaluation of the
adnexa is an advanced skill that requires appropriate training.
278
Although transabdominal ultrasound may be
used to identify these structures, transvaginal ultrasound is the preferred modality to visualize the adnexa.
The use of transvaginal ultrasound has been shown to improve physician confidence in the evaluation of
nonpregnant women with pelvic pain as compared to a traditional bimanual exam.
279
Ovarian torsion is
challenging to diagnose and is often a missed diagnosis in the ED.
280
The use of bedside ultrasound may
expedite identifying ovarian cysts, presence of venous and/or arterial blood flow, and an enlarged ovary,
which may be an early sign of torsion despite visualizing blood flow.
281
Differentiating pelvic inflammatory
disease from TOA is important for management decisions, and the sensitivity of ultrasound for the diagnosis
of tubo-ovarian abscess ranges from 56-93%, with specificity ranging from 86%-98%.
282
The use of CUS to
rapidly identify TOA may help expedite treatment.
283
Clinical US may also lead to an early diagnosis of rare
adnexal conditions such as hyperstimulation syndrome and lead to rapid treatment.
284
Advanced Echocardiography
Advanced echocardiography is beneficial in the evaluation of emergency department patients, particularly in
the critically ill when basic echocardiography is not definitive. Examples include recognizing early
tamponade physiology,
285,286
acute diastolic heart failure,
287,288
acute pulmonary embolism,
289-291
myocardial
injury in acute coronary syndrome,
292,293
and hemodynamic states like fluid tolerance and
responsiveness.
294,295
These assessments use spectral or tissue Doppler over or near valves, with calculations
based on amplitude ratios or flow pattern tracings.
Transthoracic echocardiography during cardiac arrest is another emerging application. Early literature
focused on echocardiographic cardiac standstill as a prognostic factor to discontinue resuscitation. However,
ultrasonographic determination of cardiac standstill may be difficult,
296
and more attention has been centered
around using echocardiography to guide ACLS. Obtaining views before the pulse check pause prevents
inadvertent delay over the ten second window.
297
Focusing on views of the left ventricle allows for assessment
of CPR compression location and adequacy.
298
Fine ventricular fibrillation or tachycardia appear with subtle
tremulous movements of ventricular free walls and valves.
298,299
Visualization of these shockable rhythms is
useful as they may not always appear on patient monitors. These concepts are mirrored in emerging
transesophageal literature.
Contrast-Enhanced Ultrasound
Contrast-enhanced ultrasound (CEUS) has several potential applications in the acute care setting.
300
The use
of ultrasound contrast agents (UCAs), microbubbles that are injected intravascularly, is FDA approved for
use in echocardiography and evaluation of liver lesions in adults, as well as vesicoureteral reflux evaluation
in children. UCA use in the evaluation of solid organ injury in blunt abdominal trauma is an off-label
application that is well-supported in European literature. In 2009, Catalano et al published a study of 156
patients with blunt abdominal trauma, showing ultrasound contrast improved the sensitivity of identifying
renal trauma from 36% to 69%, liver trauma from 68% to 84%, and splenic trauma from 77% to 93%.
301
Specificity of identifying injury improved from 98% to 99% in renal trauma, 97% to 99% in liver trauma,
and 96% to 99% in splenic trauma.
301
Serious adverse events occur rarely. In a study of 30,222 patients,
0.02% had an adverse reaction and 2 patients (0.007%) had early signs of anaphylaxis that improved with

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 33 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
treatment.
302
Future possible applications beyond trauma include the evaluation of abdominal aortic aneurysm
rupture, sono-thrombolysis, and assessment of tissue perfusion.
303-305
Transcranial Doppler
Transcranial Doppler (TCD) through the transtemporal window may be incorporated as an adjunct imaging
modality for the neurocritical patient. TCD may be used to evaluate for mass effect causing brain midline
shift,
306
vasospasm after subarachnoid hemorrhage (SAH),
307
diagnosis and thrombolytic efficacy in acute
ischemic stroke,
308
elevated intracranial pressure,
309
and cerebral circulatory arrest.
310
The presence and extent
of midline shift may be assessed by measuring the distance from the ipsilateral temporal bone to the midline
third ventricle, and then repeating that measurement from the contralateral temporal bone. After suffering a
SAH, vasospasm may be suggested by increased blood flow velocity in the middle cerebral artery (MCA)
due to the inverse relationship between cerebral blood vessel diameter and velocity. In the setting of acute
ischemic stroke, MCA blood flow velocities may be used to suggest the success or failure of recanalization
after thrombolysis. Lastly, detection and dynamic evaluation of elevated intracranial pressure can be
examined through the semi-quantitative relationship between systolic and diastolic blood flow velocity as
intracranial pressure rises and cerebral perfusion pressure falls. The end-stage flow patterns may serve as an
adjunct for determining cerebral circulatory arrest and brain death.
Transesophageal Echocardiography
With the same goal-directed framework of CUS applications, focused or resuscitative transesophageal
echocardiography (TEE) has been increasingly utilized for the evaluation of intubated critically-ill patients.
Several observational studies performed in the late 1990s and early 2000s demonstrated the feasibility and
clinical impact of TEE to identify reversible pathologies and guide therapies in patients with cardiac arrest
and peri-arrest states in the ED,
311
intensive care units,
312,313
and operative settings.
314-7
Subsequent studies have established that emergency physicians can obtain focused TEE images after a brief
structured simulation-based training.
318,319
In addition to the same diagnostic, prognostic, and therapy-guiding
role provided by TTE, TEE presents unique advantages in the resuscitative setting, including the ability to
obtain high-quality images regardless of body habitus, presence of subcutaneous emphysema, use
of mechanical ventilation or ongoing cardiopulmonary resuscitation (CPR). In a retrospective observational
study, Arntfield et al reported the successful implementation of a focused ED-TEE program demonstrating
that TEE was feasible, safe, and clinically influential.
320
In 78% of the exams performed, there was a
diagnostic impact on case management, which was commonly cited as excluding etiologies of cardiac arrest.
An analysis based on TEE diagnoses suggested that 55.6% of these exams had findings that could not be
easily visualized on TTE.
In a prospective observational study of out-of-hospital cardiac arrest (OHCA) patients, Teran et al found
resuscitative TEE could be performed early in the resuscitation, and found TEE to have a diagnostic, therapy-
guiding or prognostic impact in 97% of cases. Diagnoses included fine ventricular fibrillation, right
ventricular dilation, and the presence of intracardiac thrombus. In addition to the diagnostic applications of
resuscitative TEE, this modality offers the unique possibility to visualize the heart during the performance of
chest compressions, thus the potential to optimize the quality of CPR. In a prospective ED study, the hand
position used during external chest compressions resulted in compression of the left ventricular outflow tract
(LVOT) and the aortic root, but not the left ventricle (LV), and found a correlation between the area of
maximal compression (AMC) and the stroke volume (SV), where compressions closer to the LV produced
higher a SV.
320
Consistent evidence was reported in recent years by Cha et al, Teran et al, and Catena et al.
321-
323
Taken together, these studies support the idea that TEE can be used by clinicians to optimize the quality

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 34 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
of chest compressions in real time during CPR, by identifying and correcting compression of the outflow
tract, with the potential to improve outcomes.
Studies in the ED setting have also shown that TEE could shorten chest compression interruptions,
324
and
guide resuscitative procedures such as guidance of intravenous pacemaker placement,
325
and extracorporeal
membrane oxygenation (ECMO).
326,327

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 35 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
Appendix 3. Clinical Ultrasound Learning Objectives
Listed below are recommended learning objectives for a comprehensive CUS clinician curriculum, rotation,
or series of training courses. For detailed indications, limitations, protocols, documentation requirements, and
other important details for each application, please refer to the ACEP Emergency Ultrasound Imaging Criteria
Compendium.
12
Introduction
• Distinguish between consultative, clinical, point-of-care, and emergency ultrasound (EUS).
• Recognize primary CUS applications.
• Discuss support for CUS from key organizations including ACEP, AMA, ABEM, SAEM, and AIUM.
• Describe ACEP recommendations on training and credentialing in CUS.
Physics & Instrumentation
• Explain ultrasound physics relevant to CUS:
Piezoelectric effect
Frequency
Resolution
Attenuation
Echogenicity
Doppler - color and spectral
Aliasing
• Operate the EUS system as needed to obtain and interpret images adequate for clinical decision making
including:
Knobology
Image mode
Gain
Time gain compensation (TGC)
Focus
Transducer types
• Recognize common ultrasound artifacts including:
Reverberation
Side lobe
Mirror
Shadowing
Enhancement
Ring-down
Trauma (Focused Assessment by Sonography in Trauma (FAST)
• Describe the indications, clinical algorithm, and limitations of CUS in blunt and penetrating
thoracoabdominal trauma.
• Perform the CUS protocol for Trauma in both primary and secondary surveys.
• Identify relevant US anatomy including the pleura, diaphragm, inferior vena cava, pericardium, liver,
spleen, kidneys, bladder, prostate and uterus.
• Recognize pathologic findings and pitfalls in the evaluation of pneumothorax, hemothorax, pulmonary
contusion, hemopericardium, cardiac activity, volume status, and hemoperitoneum.
• Integrate Trauma CUS findings into individual patient, departmental, and disaster management.
Female Pelvis
• Transabdominal and/or transvaginal approach

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 36 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
• Basic obstetrical CUS
First-Trimester Pregnancy
• Describe the indications, clinical algorithm, and limitations of CUS in first-trimester pregnancy pain
and bleeding.
• Understand the utility of quantitative B-HCG in the evaluation of first-trimester pregnancy pain and
bleeding.
• Perform CUS protocols for transabdominal and transvaginal views as appropriate, including fetal heart
rate and gestational age measurement techniques.
• Identify relevant US anatomy including the cervix, uterus, adnexa, bladder and cul-de-sac.
• Recognize the relevant findings and pitfalls when evaluating for intrauterine and ectopic pregnancy:
- Early embryonic structures including the gestational sac, yolk sac, fetal pole, and heart
- Location of embryonic structures in pelvis
- Embryonic demise
- Molar pregnancy
- Findings of ectopic pregnancy including pseudogestational sac, free fluid, and adnexal masses
Advanced Evaluation
• Basic gynecological CUS
• Ovarian cysts, fibroids, tubo-ovarian abscesses
• Ovarian torsion
• Ectopic pregnancy
• 2
nd
and 3
rd
trimester OB
• Integrate pregnancy EUS findings into individual patient and departmental management.
Aorta
• Describe indications, clinical algorithm, and limitations of CUS in the evaluation of abdominal and
thoracic aortic pathology.
• Perform CUS protocols to evaluate the abdominal and thoracic aorta including measurement
techniques.
• Identify relevant US anatomy including the aorta with major branches, inferior vena cava, and vertebral
bodies.
• Recognize pathologic findings and pitfalls when evaluating for abdominal and thoracic aortic aneurysm
and dissection.
• Integrate Aorta EUS findings into individual patient and departmental management.
Cardiac and Hemodynamic Assessment
• Describe the indications and limitations of cardiac CUS.
• Perform standard CUS windows (subcostal, parasternal, and apical) and planes (four chamber, long
and short axis).
• Identify relevant US anatomy including pericardium, cardiac chambers, valves, descending aorta and
inferior vena cava.
• Estimate qualitative left ventricular function and central venous pressure to guide hemodynamic
assessment of patient.
• Recognize cardiac arrest, pericardial effusions with or without tamponade, and dilation of the aortic
root or the descending aorta.
• Advanced evaluation
- Acquire view of the aortic arch and recognize aortic arch dissection and/or aneurysm.
- Identification of right ventricular dysfunction.
- Assessment of cardiac output and fluid responsiveness.

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 37 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
• Procedural guidance: pericardiocentesis, transvenous pacer, and central venous catheter placement
• Integrate Emergency echocardiography findings into individual patient and departmental management.
Hepatobiliary
• Describe the indications and limitations of CUS of the biliary tract.
• Perform CUS protocols to evaluate the biliary tract.
• Identify relevant ultrasound (US) anatomy including the gallbladder, portal triad, inferior vena cava,
and liver.
• Recognize the relevant findings and pitfalls when evaluating for cholelithiasis and cholecystitis.
• Advanced evaluation
- Common bile duct pathology (dilatation and choledocholithiasis)
- Liver pathology (masses, pneumobilia, hepatomegaly)
- Portal vein abnormalities
- Pancreas pathology
• Integrate EUS of the biliary tract into individual patient and departmental management.
Urinary Tract
• Describe the indications and limitations of CUS of the kidneys and bladder.
• Perform CUS protocols to evaluate the urinary tract.
• Identify relevant US anatomy including the renal cortex, renal pelvis, ureter, bladder, liver, spleen, and
uterus or prostate.
• Recognize the relevant findings and pitfalls when evaluating for hydronephrosis, renal calculi, renal
masses, bladder volume, pregnancy, and Foley catheter evaluation.
• Integrate EUS of the urinary tract into individual patient and departmental management.
Deep Vein Thrombosis
• Describe the indications and limitations of CUS for the detection of deep venous thrombosis.
• Understand the differences between lower extremity venous CUS and radiology lab-or vascular lab-
performed “Duplex evaluation”
• Perform CUS protocols for the detection of deep venous thrombosis of the upper and lower extremities
including:
- Vessel identification
- Compression
- Doppler imaging of respiratory variation and augmentation.
• Identify relevant US anatomy of the upper and lower extremities including the deep venous and arterial
systems, major nerves, and lymph nodes.
• Recognize the relevant findings and pitfalls when evaluating for deep venous thrombosis.
• Integrate EUS for deep venous thrombosis into individual patient and departmental management.
Skin and Soft Tissue
• Describe the indications and limitations of skin and soft tissue EUS.
• Perform EUS protocols for the evaluation of skin and soft tissue pathology.
• Identify relevant US anatomy including:
- Skin
- Adipose
- Lymph Nodes
• Recognize the relevant findings and pitfalls when evaluating the following:
- Soft tissue infections: Abscess versus cellulitis
- Subcutaneous fluid collection identification
- Foreign body location and removal

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 38 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
• Integrate skin and soft tissue EUS findings into individual patient and departmental management.
Musculoskeletal
• Describe the indications and limitations of musculoskeletal EUS.
• Perform EUS protocols for the evaluation of musculoskeletal pathology.
• Identify relevant US anatomy including:
- Tendons and Ligaments
- Muscles
- Bones
- Joints
• Recognize the relevant findings and pitfalls when evaluating the following:
- Tendon injury (laceration, rupture)
- Fractures
- Joint identification
• Integrate musculoskeletal EUS findings into individual patient and departmental management.
Thoracic/Airway
• Describe the indications and limitations thoracic CUS
• Perform CUS protocols for the detection of:
- Pneumothorax
- Pleural Effusion
- Interstitial Lung Fluid (CHF, ARDS, pneumonia, pulmonary contusion)
• Identify relevant US anatomy of thoracic structures.
• Recognize the relevant findings and pitfalls when evaluating for thoracic pathology
• Recognize the sonographic findings of tracheal and esophageal anatomy, especially in regard to EM
procedures
• Integrate thoracic CUS findings into individual patient and departmental management.
Ocular
• Describe the indications, limitations, and relative contraindications of ocular CUS.
• Perform CUS protocols for the detection of
- Vitreous hemorrhage
- Posterior vitreous detachment
- Retinal detachment
- Optic nerve sheath diameter measurement
- Optic disc evaluation
• Advanced evaluation
- Lens pathology
- Foreign body
- Globe rupture
- Retrobulbar hematoma
- Central retinal artery/vein occlusion
- Subretinal hemorrhage
• Light reflex
- Identify relevant US anatomy of the globe and orbital structures.
- Recognize the relevant findings and pitfalls when evaluating for ocular pathology.
• Integrate ocular CUS into individual patient and departmental management.

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 39 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
Procedural Guidance
• Describe the indications and limitations when using US guidance for bedside procedures.
• Perform CUS protocols for procedural guidance including both transverse and longitudinal approaches
when appropriate. These procedures may include:
- Vascular access: Central and peripheral
- Confirmation of endotracheal intubation
- Pericardiocentesis
- Paracentesis
- Thoracentesis
- Foreign body detection and removal
- Evaluation and aspiration/drainage of body fluid
- Arthrocentesis
- Pacemaker placement and capture
- Abscess identification and drainage
- Regional anesthesia
• Identify relevant US anatomy for each particular procedure.
• Recognize the relevant findings and pitfalls when performing CUS for procedural guidance.
• Integrate CUS for procedural guidance into individual patient and departmental management.
Bowel
• Describe the indications and limitations of bowel CUS
• Perform CUS protocols for the detection of:
- Acute appendicitis
- Small and Large Bowel obstruction
- Pneumoperitoneum
- Diverticulitis
- Hernia
- Intussusception and Pyloric Stenosis
- Evaluation/placement of orogastric/nasogastric or percutaneous gastronomy tube
• Identify relevant US anatomy of bowel structures.
• Recognize the relevant findings and pitfalls when evaluating for bowel pathology
• Integrate bowel CUS findings into individual patient and departmental management.
Transesophageal Echocardiography (TEE)
• Describe the indications, limitations, and contraindications to resuscitative TEE.
• Perform standard TEE views to evaluate for cardiac pathology, guidance of chest compressions in
cardiopulmonary resuscitation, and procedures, such as pericardiocentesis, pacemaker placement, and
ECMO catheter placement.
• Advanced evaluation:
- Regional wall motion abnormalities
- Aortic dissection
- Aortic aneurysm

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 40 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
Appendix 4. Recommendations for an EM Residency CUS Education Program
Successful EUS Residency Education in accordance with these guidelines requires significant departmental
and institutional support. The purpose of these additional recommendations is to delineate the scope of
resources required to facilitate the development and maintenance of CUS Residency Education programs.
Application of these recommendations is dependent on EM residency size, current and planned CUS
utilization, and institutional capabilities.
CUS Faculty:
1. CUS Director: At least one full time EM attending faculty with sufficient CUS program coordination
expertise. Sufficient non-clinical time for planning and conducting all CUS program activities is essential
to ensuring adequate resident training.
2. CUS Faculty: At least one additional full time EM attending faculty member committed to actively
developing CUS expertise. Sufficient non-clinical time for conducting CUS program activities is essential
to ensuring adequate resident training. The number of dedicated CUS faculty needed is dependent on the
size of the residency and quality of the training program desired.
3. Credentialed CUS Faculty: To adequately supervise and educate residents in CUS, a minimum of fifty
percent of Core Faculty members at all EM residency programs need to be credentialed in CUS. For
example, if a program has 12 core faculty, then 6 need to be credentialed in CUS. May be inclusive of
the CUS Director and Faculty.
Equipment and Materials:
1. CUS systems with appropriate transducers and imaging capabilities readily available for immediate
resident clinical use 24/7.
2. CUS educational (online and/or print) resources readily available for access.
3. Recent and landmark CUS literature as well as opportunities to participate in local quality improvement
and research projects need to be provided to residents and core US faculty.
Curriculum Components and Competency Assessment:
1. Initial CUS Training: Didactic and hands-on instruction in CUS physics, machine use, and introduction
to core CUS applications need to be provided early in residency as a half or full day course.
2. Annual CUS Rotations: Two-week rotation in the first year to learn basic EUS knowledge and skills,
followed by at least one week in each subsequent year to reinforce learning and acquire more advanced
skills. One rotation without continued learning within the EM residency curriculum is inadequate. For
each trainee, a minimum of 80 hours of dedicated EUS rotation time is recommended during an EM
residency.
3. Suggested rotation educational methods and assessment measures:
a. Orientation: Begin rotation with a baseline CUS skills assessment to identify trainee’s unique
learning needs. Follow with hands-on small group instruction in the ED focusing on machine
operation, exam protocols, image optimization and interpretation, documentation, as well as
integration of CUS findings into daily clinical practice.
b. Scheduled supervised scanning shifts with CUS faculty in the ED to provide opportunities for both
proctored and semi-independent image acquisition and interpretation. All training exams are
submitted for timely quality assurance review.
c. Weekly Academic Day:
i. Quality Assurance/Improvement Review session during which a portion of current trainee’s
CUS exams are discussed, focusing on challenging cases, pathology, and integration into daily
patient and ED management.
ii. Simulation cases and review of image libraries for additional exposure to less common
pathology.
ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 41 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
iii. Journal club including a discussion of a recent or landmark CUS literature, an online narrated
didactic or live lecture, or chapter review.
iv. Hands-on small group instruction in the ED focusing on current trainees learning needs
identified during QA/QI Review or scanning shifts.
d. End the rotation with a final assessment of CUS knowledge utilizing a standardized exam such as the
ACEP US Online Exams, as well as an additional CUS skill assessment.
e. Provide a timely end of CUS rotation assessment of knowledge and skills to each resident.
Additionally, provide trainees with continued opportunities to evaluate the CUS program itself.
4. Achieving CUS exam requirements: Completion of set number examinations documents adequate
experience to develop proficiency. Additional assessment measures described in these guidelines are
needed to ensure CUS competency such as participation in QA/QI sessions, SDOTs, OSCEs, and
simulation assessments. CUS directors can certify CUS training at the end of residency.
5. Ongoing Quality Assurance System: Digital archiving system for CUS exam images and interpretations
for timely quality assurance review and trainee feedback on individual exams which includes technique
and image interpretation.
a. All trainee exams need to be reviewed by CUS faculty until minimum benchmarks are achieved.
After this, a proportion of trainee exams need to be reviewed on an ongoing basis throughout
residency.
b. Timely exam feedback must be provided to trainees during and between CUS rotations. Trainees
need ready access to individual exam feedback and total exams completed by application and overall.
6. Integrated CUS training in the residency curriculum: Learning needs to be reinforced during quarterly or
biannual EUS workshops comprised of CUS didactics and hands-on instruction. An additional 20 hours
of dedicated CUS learning between rotations is recommended during a 3 or 4 year residency.

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 42 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
Appendix 5. Recommendations for a CUS Course
Successful training courses in CUS require significant advance planning and resource commitment. The
curriculum designed by the course director should include a trainee needs assessment, educational learning
objectives, educational methods, and assessment measures. The learning objectives for any CUS Course or
rotation are listed in Appendix 3. Important considerations are discussed below
1. Faculty: The course director must be a physician and known expert in clinical ultrasound. The course
director should recruit other clinicians already credentialed in CUS to assist with knowledge learning,
skills training, and trainee assessment. Several faculty planning meetings are recommended during
curriculum development as well as a meeting immediately prior to the course to provide all faculty with
an understanding of the setup, curriculum, and logistics.
2. Site and Set Up: The ideal course site includes a large didactic room as well as separate rooms or areas
for scanning stations. Private areas for endovaginal US are required if this topic will be covered during
training.
a. Ultrasound Stations: Appropriate machines and transducers are necessary. The learner to instructor
ratio should be no higher than 5 to 1 to ensure appropriate skills training.
b. Ultrasound Models: Image acquisition protocols may be learned on normal live models. Image
interpretation requires the incorporation of patients with known pathologic findings, simulators, or
incorporation of image libraries.
i. Pathology models may include otherwise healthy paid or volunteer persons with pericardial
effusions, cholelithiasis, aortic aneurysms and chronic ambulatory peritoneal dialysis patients.
ii. Full informed consent should be obtained from all models and a signed waiver of responsibility
is recommended. If an undiagnosed finding is discovered in a model, then the course director
must appropriately notify the model and ensure appropriate follow up.
3. Knowledge Learning:
a. An introductory course for trainees must include instruction in basic US physics, machine operation,
and a small number of initial CUS applications to be clinically utilized. Suggested initial applications
include Trauma Ultrasound, Central and Peripheral Venous Access, and Abdominal Aortic
Aneurysm ultrasound. However, the initial applications will vary by local site as determined by a pre-
course needs assessment completed by the course director and local trainee leadership.
i. A half-day introductory course is appropriate for a single application. Longer courses are
required for additional applications. Shorter, repeated courses, supplemented by routine, quality
assured, CUS performance during clinical work, are more likely to improve learning and
utilization.
b. Pre- and post-course educational materials must be provided to reinforce course learning. Suggested
sources of information include course director approved online narrated lectures, podcasts, websites,
traditional textbooks, didactic syllabi, and journal articles.
i. Utilization of the flipped classroom provides the opportunity for more focused didactics
reviewing key concepts and answering trainee questions at the course. Focused didactics provide
the opportunity for increased skill training.
ii. Frequent rotations between didactics and skills training sessions improve trainee and faculty
engagement.
4. Skills Training:
The technical laboratory is an integral component of any ultrasound course.

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 43 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
a. Based on the needs assessment, appropriate and specific learning objectives need to be defined for
each station.
i. Trainees should be deliberately assigned to small groups not necessarily including immediate
peers to create more focused learning teams.
ii. For trainees with prior CUS experience, an initial skills assessment with an SDOT or simulator
will help to ensure that trainee specific instruction is provided.
iii. Instructors should work to maximize the time that the transducer is the trainee's’ hands, avoid
over teaching of advanced concepts beyond the trainees needs, encourage questions, and
consistently engage each trainee.
ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 44 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
Appendix 6. CUS Training for Medical Students
CUS Training during a one-month EM Rotation:
General EM clerkships should include an introduction to CUS that may entail a single dedicated clinical US
shift with direct faculty supervision, a one-day CUS course, or simply case-by-case incorporation of CUS
into patient care in the ED. Students should strive to become familiar with a single CUS application such as
the FAST exam, and should be exposed to additional CUS exams over the course of the clerkship. CUS
literature, selected textbook chapters, online modules or digital resources should be made available for
student review.
Dedicated CUS rotation recommendations:
1. Emergency US and CUS rotations should begin with instruction in Physics/Instrumentation, followed
by select applications such as FAST, Aorta, Renal, Hepatobiliary Cardiac, Procedures, Pelvic (including
endovaginal US), Deep Venous Thrombosis, Skin and Soft Tissue, and Musculoskeletal.
2. Didactic education should be delivered in electronic, preferably online, format in an attempt to maximize
hands-on education in the clinical area. A reliable resource that course directors may choose to utilize
for US didactic material is the ACEP Sonoguide website. available on the ACEP Web site
(www.acep.org/sonoguide).
3. Assessments should include a pre-test including still image/video interpretation and case-based
applications of CUS. To assess their progress, the same test may be completed at the end of the rotation.
4. Each student should obtain between 75 to 100 scans over the course of a 4-week rotation, or
approximately 40-50 scans over the course of a 2-week rotation. Dedicated shifts may include evenings
or weekends to maximize exposure to pathology and interesting emergency US cases. If digital tracking
is not available, students should generate a personal log of CUS exams on which to build during their
postgraduate education.
5. All student-performed scans should be directly supervised by CUS credentialed faculty or recorded for
subsequent quality assurance review with the rotation director or adjunct ultrasound faculty.
6. Students should complete the reading of an assigned CUS text or viewing of an assigned online
curriculum over the course of the rotation. In addition, it is recommended that students identify a current
publication relevant to CUS to discuss their findings with the rotation director.
Additional Opportunities for CUS Training in Undergraduate Medical Education:
With the advent of more US in various specialties, this preparation in medical school can benefit students
with interests outside of emergency medicine.
Emergency and Clinical US directors could consider incorporating US into:
1. Gross anatomy course highlighting common US anatomy (eg, FAST exam during study of the
abdomen, heart)
2. Physiology course highlighting doppler, M mode, and basic waveform analysis.
3. Pathology course highlighting common pathologies such as fluid in potential spaces, depressed cardiac
function, cellulitis, abscess, retinal detachment or other commonly seen pathologies in the ED.
4. Introduction to Clinical Medicine course highlighting US guided vascular access.
5. Ultrasound in the physical exam. Although US use in clinical practice is a diagnostic test that warrants
a generated report, it can be used to teach components of the physical exam. For example, teaching the
traditional cardiac auscultation can be augmented with cardiac images of the heart.
6. Ultrasound training before clinical rotations. Some schools have developed short clinical skills time
before rotations where US can be implemented to help student learners see how US is used in that
particular field.
7. Ultrasound electives in the 4th year can include a longitudinal program where US lectures, hands on,
and journal club can be incorporated into a course.

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 45 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
The future of US in medical education is constantly being built, modified and ever evolving. Though it seems
like there are early adopters trying to implement CUS in medical education. one of the key components is
finding an US champion to spearhead CUS into the undergraduate medical education framework. From
there, getting students involved through an US interest group can improve the impact through direct feedback
and student motivation. The two methods of a top-down administrative implementation of US in medical
education are the best method, yet warrants buy in from the dean and the curriculum committee. A bottom
up approach through student interest, electives and extracurricular exposure takes longer but can still impact
student competence in US.

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 46 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
ACEP Emergency Ultrasound Section Writing Committee and Contributors:
Editors: Arun Nagdev MD; Penelope C. Lema, MD, FACEP; Javier E. Rosario MD, FACEP; Elaine Situ-
LaCasse, MD; and Michael Gottlieb, MD, FACEP
Introduction: Arun Nagdev MD; Penelope C. Lema, MD, FACEP; Michael Gottlieb, MD, FACEP
Scope of Practice: Vivek S. Tayal, MD, FACEP; Christopher C. Raio, MD, FACEP
Training: John M. Bailitz, MD, FACEP; Stephen J. Leech, MD, FACEP; Romolo J. Gaspari, MD, PhD,
FACEP
Credentialing: Robert A. Jones, DO, FACEP; Thompson Kehrl, MD, FACEP; Romolo J. Gaspari MD,
PhD, FACEP
Quality Assurance: J. Matthew Fields, MD, FACEP
Value and Reimbursement: Romolo J. Gaspari, MD, PhD, FACEP and Michael Gottlieb, MD, FACEP
Institutional Leadership: Resa Lewiss MD; Gerardo C. Chiricolo, MD, FACEP
Future issues: Srikar R. Adhikari MD, MS, FACEP
Core and Advanced Applications: Lindsay A. Taylor MD, FACEP; Megan Leo, MD; Judy C. Lin MD,
FACEP; Sara Damewood, MD, FACEP; Frances Russell, MD, FACEP; Dan Mantuani MD; Di
Coneybeare, MD, MHPE; Amy Marks MD; Josie G. Acuña MD; Stephen Alerhand, MD; Petra Duran-
Gehring, MD, FACEP; Margaret Lin-Martore, MD; Lori A. Stolz, MD, FACEP; Rachel B. Liu MD,
FACEP; Felipe Teran, MD, FACEP; Laura Oh MD, FACEP; Michael Gottlieb MD, FACEP.
References
1. Chiu L, Jairam MP, Chow R, et al. Meta-analysis of point-of-care lung ultrasonography versus chest
radiography in adults with symptoms of acute decompensated heart failure. Am J Cardiol.
2022;174:89-95.
2. Fields JM, Davis J, Alsup C, et al. Accuracy of point-of-care ultrasonography for diagnosing acute
appendicitis: A systematic review and meta-analysis. Acad Emerg Med. 2017;24(9):1124-36.
3. Gottlieb M, Patel D, Marks A, Peksa GD. Ultrasound for the diagnosis of shoulder dislocation and
reduction: A systematic review and meta-analysis. Acad Emerg Med. 2022;29(8):999-1007.
4. Tran QK, Fairchild M, Yardi I, Mirda D, Markin K, Pourmand A. Efficacy of ultrasound-guided
peripheral intravenous cannulation versus standard of care: A systematic review and meta-analysis.
Ultrasound Med Biol. 2021;47(11):3068-78.
5. Gu WJ, Wu XD, Wang F, Ma ZL, Gu XP. Ultrasound guidance facilitates radial artery
catheterization: A meta-analysis with trial sequential analysis of randomized controlled trials. Chest.
2016;149(1):166-79.
6. Gottlieb M, Holladay D, Peksa GD. Ultrasound-assisted lumbar punctures: A systematic review and
meta-Analysis. Acad Emerg Med. 2019;26(1):85-96.
ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 47 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
7. Heller MB, Mandavia D, Tayal VS, et al. Residency training in emergency ultrasound: fulfilling the
mandate. Acad Emerg Med. 2002;9:835-9.
8. ACR-SPR-SRU Practice Parameter for Performing and Interpreting Diagnostic Ultrasound
Examinations. 2017. Accessed December 2022 at https://www.acr.org/-/media/ACR/Files/Practice-
Parameters/us-perf-interpret.pdf
9. ACEP Emergency Ultrasound Section. Emergency Ultrasound Coding and Reimbursement
Document. 2021. Accessed December 2022 at
https://www.acep.org/emultrasound/subcommittees/coding-reimbursement/
10. Geria RN, Raio CC, Tayal V. Point-of-care ultrasound: not a stethoscope-a separate clinical entity. J
Ultrasound Med. 2015;34:172-3.
11. American College of Emergency Physicians. Definition of Clinical Ultrasonography [policy
statement]. Reaffirmed June 2022. Accessed December 2022 at https://www.acep.org/patient-
care/policy-statements/definition-of-clinical-ultrasonography
12. American College of Emergency Physicians. Emergency Ultrasound Imaging Criteria Compendium
[policy statement]. Approved October 2021. Accessed December 2022 at
https://www.acep.org/patient-care/policy-statements/Emergency-Ultrasound-Imaging-Criteria-
Compendium/
13. Shah VP, Tunik MG, Tsung JW. Prospective evaluation of point-of-care ultrasonography for the
diagnosis of pneumonia in children and young adults. JAMA Pediatr. 2013;167:119-25.
14. Gallagher RA, Levy J, Vieira RL, et al. Ultrasound assistance for central venous catheter placement
in a pediatric emergency department improves placement success rates. Acad Emerg Med.
2014;21:981-6.
15. Elikashvili I, Tay ET, Tsung JW. The effect of point-of-care ultrasonography on emergency
department length of stay and computed tomography utilization in children with suspected
appendicitis. Acad Emerg Med. 2014;21:163-70.
16. Bartocci M, Fabrizi G, Valente I, et al. Intussusception in childhood: role of sonography on diagnosis
and treatment. J Ultrasound. 2015;18:205-11.
17. Plumb J, Mallin M, Bolte RG. The role of ultrasound in the emergency department evaluation of the
acutely painful pediatric hip. Pediatr Emerg Care. 2015;31:54-8; quiz 9-61.
18. Deanehan J, Gallagher R, Vieira R, et al. Bedside hip ultrasonography in the pediatric emergency
department: a tool to guide management in patients presenting with limp. Pediatr Emerg Care.
2014;30:285-7.
19. Marin JR, Lewiss RE, AAP, et al. Point-of-care ultrasonography by pediatric emergency medicine
physicians. Pediatrics. 2015;135(4):e1113-22.
20. Vieira RL, Hsu D, Nagler J, et al. Pediatric emergency medicine fellow training in ultrasound:
consensus educational guidelines. Acad Emerg Med. 2013;20:300-6.
21. Zieleskiewicz L, Muller L, Lakhal K, et al. Point-of-care ultrasound in intensive care units:
assessment of 1073 procedures in a multicentric, prospective, observational study. Intensive Care
Med. 2015;41:1638-47.
22. Gallard E, Redonnet JP, Bourcier JE, et al. Diagnostic performance of cardiopulmonary ultrasound
performed by the emergency physician in the management of acute dyspnea. Am J Emerg Med.
2015;33:352-8.
23. Nelson BP, Sanghvi A. Out of hospital point of care ultrasound: current use models and future
directions. Eur J Trauma Emerg Surg. 2016;42:139-50.
24. Press GM, Miller SK, Hassan IA, et al. Evaluation of a training curriculum for prehospital trauma
ultrasound. J Emerg Med. 2013;45:856-64.

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 48 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
25. Taylor J, McLaughlin K, McRae A, et al. Use of prehospital ultrasound in North America: a survey of
emergency medical services medical directors. BMC Emerg Med. 2014;14:6.
26. Shorter M, Macias DJ. Portable handheld ultrasound in austere environments: use in the Haiti
disaster. Prehosp Disaster Med. 2012;27:172-7.
27. Zhou J, Huang J, Wu H, et al. Screening ultrasonography of 2,204 patients with blunt abdominal
trauma in the Wenchuan earthquake. J Trauma Acute Care Surg. 2012;73:890-4.
28. Zhang S, Zhu D, Wan Z, et al. Utility of point-of-care ultrasound in acute management triage of
earthquake injury. Am J Emerg Med. 2014;32:92-5.
29. Raja AS, Propper BW, Vandenberg SL, et al. Imaging utilization during explosive multiple casualty
incidents. J Trauma. 2010;68:1421-4.
30. Shah S, Dalal A, Smith RM, et al. Impact of portable ultrasound in trauma care after the Haitian
earthquake of 2010. Am J Emerg Med. 2010;28:970-1.
31. Kirkpatrick AW, Campbell MR, Novinkov OL, et al. Blunt trauma and operative care in
microgravity: a review of microgravity physiology and surgical investigations with implications for
critical care and operative treatment in space. J Am Coll Surg. 1997;184:441-53.
32. Campbell MR, Billica RD, Johnston SL, et al. Performance of advanced trauma life support
procedures in microgravity. Aviat Space Environ Med. 2002;73:907-12.
33. Russell TC, Crawford PF. Ultrasound in the austere environment: a review of the history, indications,
and specifications. Mil Med. 2013;178:21-8.
34. Rozanski TA, Edmondson JM, Jones SB. Ultrasonography in a forward-deployed military hospital.
Mil Med. 2005;170:99-102.
35. Morgan AR, Vasios WN, Hubler DA, et al. Special operator level clinical ultrasound: an experience
in application and training. J Spec Oper Med. 2010;10:16-21.
36. Strode CA, Rubal BJ, Gerhardt RT, et al. Satellite and mobile wireless transmission of focused
assessment with sonography in trauma. Acad Emerg Med. 2003;10:1411-4.
37. Bahner DP, Goldman E, Way D, Royall NA, Liu YT. The state of ultrasound education in U.S.
medical schools: results of a national survey. Acad Med. 2014;89:1681-6.
38. Soni NJ, Schnobrich D, Matthews BK, Tierny DM, Jensen TP, Dancel R, et al. Point-of-Care
Ultrasound for Hospitalists: A Position Statement of the Society of Hospital Medicine. J Hosp Med.
2019;14:E1–E6.
39. Beal EW, Sigmond BR, Sage-Silski L, Lahey S, Nguyen V, Bahner DP. Point-of-care ultrasound in
general surgery residency training: A proposal for milestones in graduate medical education
ultrasound. J Ultrasound Med. 2017;36:2577-84.
40. Young AC, Butts C, deBoisblanc BP, Tejedor RS, Kantrow SP, Lammi MR. Implementation of a
longitudinal critical care fellowship ultrasound curriculum. ATS Scholar. 2022;3:125-34.
41. Smalley CM, Fertel BS, Broderick E. Standardizing point-of-care ultrasound credentialing across a
large health care system. Jt Comm J Qual Patient Saf. 2020;46:471-6.
42. Bahner DP, Hughes D, Royall NA. I-AIM: a novel model for teaching and performing focused
sonography. J Ultrasound Med. 2012;31:295-300.
43. Damewood SC, Leo M, Bailitz J, Gottlieb M, Liu R, Hoffmann B, et al. Tools for measuring clinical
ultrasound competency: recommendations from the Ultrasound Competency Work Group. AEM Educ
Train. 2020;4:S106-S112.
44. Panebianco NL, Liu RB, Alerhand S, Au AK, Bailitz J, Chiem AT, et al. Joint recommendations and
resources for clinical ultrasound education amidst the COVID-19 era. AEM Educ Train. 2020;4:438-
42.
45. Smalley CM, Browne V, Kaplan B, Russ B, Wilson J, Lewiss RE. Early innovative immersion: a
course for pre-medical professions students using point-of-care ultrasound. J Ultrasound Med.
2016;35:2681-6.

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 49 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
46. Smalley CM, Sande M, Wilson J, Lewiss RE. An education innovation to improve point-of-care
ultrasound skills in senior emergency medicine residents: a mandatory advanced rotation. J Medic
Educ Training. 2017;1:001.
47. American College of Emergency Physicians. Sonoguide. Accessed December 2022:
https://www.acep.org/sonoguide/
48. Society for Academic Emergency Medicine Academy for Emergency Ultrasound Asynchronous
Ultrasound Curriculum. In: Default [Internet]. Accessed December 2022. Available:
https://www.saem.org/about-saem/academies-interest-groups-affiliates2/aeus/education/aeus-off-the-
shelf-asynchronous-ultrasound-curriculum
49. Miller GT, Scerbo MW, Zybak S, Byars DV, Goodmurphy CW, Lattanzio FA, et al. Learner
improvement from a simulation-enhanced ultrasonography curriculum for first-year medical students.
J Ultrasound Med. 2017;36:609-19.
50. Damewood SC, Lewiss RE, Huang JV. Ultrasound simulation utilization among point of care
ultrasound users: Results of a survey. J Clin Ultrasound. 2018;46:571-4.
51. Smith S, Lobo V, Anderson KL, Gisondi MA, Sebok‐Syer SS, Duanmu Y. A randomized control trial
of simulation‐based mastery learning to teach the extended focused assessment with sonography in
trauma. AEM Educ Train. 2021. doi:10.1002/aet2.10606
52. Harel-Sterling M, McLean LJ. Development of a blended learning curriculum to improve POCUS
education in a pediatric emergency medicine training program. CJEM. 2022;24:325-8.
53. Stolz LA, Amini R, Situ-LaCasse E, Acuña J, Irving SC, Friedman L, et al. Multimodular ultrasound
orientation: residents’ confidence and skill in performing point-of-care ultrasound. Cureus.
2018;10:e3597.
54. Lewiss RE, Hayden GE, Murray A, Liu YT, Panebianco N, Liteplo AS. SonoGames: an innovative
approach to emergency medicine resident ultrasound education. J Ultrasound Med. 2014;33:1843-9.
55. Liteplo AS, Carmody K, Fields MJ, Liu RB, Lewiss RE. SonoGames: Effect of an innovative
competitive game on the education, perception, and use of point-of-care ultrasound. J Ultrasound
Med. 2018;37:2491-6.
56. PoSaw LL, Wubben BM, Bertucci N, Bell GA, Healy H, Lee S. Teaching emergency ultrasound to
emergency medicine residents: a scoping review of structured training methods. J Am Coll Emerg
Physicians Open. 2021;2:e12439.
57. Duanmu Y, Henwood PC, Takhar SS, Chan W, Rempell JS, Liteplo AS, et al. Correlation of OSCE
performance and point-of-care ultrasound scan numbers among a cohort of emergency medicine
residents. Ultrasound J. 2019;11(1):3.
58. Anders Ericsson K. Deliberate practice and acquisition of expert performance: A general overview.
Acad Emerg Med. 2008;15:988-94.
59. Saxena M, Tan TX, Duanmu Y, Ashenburg N, Ghaziaskar Z. Seeing (virtually) is believing: The
utility of teleultrasound education for the focused assessment with sonography for trauma exam. Acad
Emerg Med. 2021;S403-S403.
60. Young K, Moon N, Wilkinson T. Building point-of-care ultrasound capacity in rural emergency
departments: An educational innovation. Can J Rural Med. 2021;26:169-175.
61. Narang A, Bae R, Hong H, Thomas Y, Surette S, Cadieu C, et al. Utility of a deep-learning algorithm
to guide novices to acquire echocardiograms for limited diagnostic use. JAMA Cardiol. 2021;6:624-
32.
62. Adhikari S, Amini R, Stolz L, O’Brien K, Gross A, Jones T, et al. Implementation of a novel point-
of-care ultrasound billing and reimbursement program: fiscal impact. Am J Emerg Med. 2014;32:592-
5.
63. Beeson MS, Carter WA, Christopher TA, Heidt JW, Jones JH, Meyer LE, et al. The development of
the emergency medicine milestones. Acad Emerg Med. 2013;20:724-9.
64. Lewiss RE, Pearl M, Nomura JT, Baty G, Bengiamin R, Duprey K, et al. CORD-AEUS: consensus
document for the emergency ultrasound milestone project. Acad Emerg Med. 2013;20:740-5.
ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 50 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
65. Cooney RR, Murano T, Ring H, Starr R, Beeson MS, Edgar L. The Emergency Medicine Milestones
2.0: Setting the stage for 2025 and beyond. AEM Educ Train. 2021;5:e10640.
66. Russell FM, Kennedy SK, Rood LK, Nti B, Herbert A, Rutz MA, et al. Design and implementation of
a basic and global point of care ultrasound (POCUS) certification curriculum for emergency medicine
faculty. Ultrasound J. 2022;14:10.
67. Budhram G, Elia T, Rathlev N. Implementation of a successful incentive-based ultrasound
credentialing program for emergency physicians. West J Emerg Med. 2013;14:602-8.
68. American College of Emergency Physicians. Guidelines Regarding the Role of Physician Assistants
and Nurse Practitioners in the Emergency Department [policy statement]. Approved March 2022.
69. Strony R, Marin JR, Bailitz J, Dean AJ, Blaivas M, Tayal V, et al. Systemwide clinical ultrasound
program development: An expert consensus model. West J Emerg Med. 2018;19:649-53.
70. Accrediting Advanced Emergency Ultrasound Fellowships. In: Emergency Ultrasound Fellowship
Accreditation Council – [Internet]. [cited 29 Apr 2022]. Available: https://eufacouncil.org/
71. Advanced EM Ultrasonography. In: American Board of Emergency Medicine [Internet]. [cited 29
Apr 2022]. Available: https://www.abem.org/public/become-certified/focused-practice-
designation/advanced-em-ultrasonography
72. Gottlieb M, Duran-Gehring P, Coneybeare D, Lema P. Creation of a novel course for the advanced
emergency medicine ultrasound focused practice designation examination. AEM Educ Train.
2022;6(5):e10810.
73. Davis JJ, Wessner CE, Potts J, Au AK, Pohl CA, Fields JM. Ultrasonography in Undergraduate
Medical Education: A Systematic Review. J Ultrasound Med. 2018;37:2667-79.
74. American Medical Association. H-230.960 Privileging for Ultrasound Imaging. Accessed December,
7, 2022, at https://policysearch.ama-
assn.org/policyfinder/detail/privileging%20for%20ultrasound%20imaging?uri=%2FAMADoc%2FH
OD.xml-0-1591.xml
75. American College of Emergency Physicians. Emergency Ultrasound Certification by External
Entities [policy statement]. Reaffirmed February 2020. Accessed December 2022 at
https://www.acep.org/patient-care/policy-statements/emergency-ultrasound-certification-by-external-
entities
76. OPPE and FPPE: Tools to help make privileging decisions. The Joint Commission, 2020. Accessed
December 2022, at https://www.jointcommission.org/standards/standard-faqs/hospital-and-hospital-
clinics/medical-staff-ms/000002291/
77. American College of Emergency Physicians. ACEP Emergency Ultrasound Standard Reporting
Guidelines [Internet]. 2018 [cited 2022 Apr 28]. Available from:
https://www.acep.org/globalassets/uploads/uploaded-files/acep/clinical-and-practice-
management/policy-statements/information-papers/emergency-ultrasound-standard-reporting-
guidelines---2018.pdf
78. Byrne M, Geria R, Kummer T, Leech S, Lewiss R, Noble V, et al. Emergency ultrasound: workflow
white paper. ACEP [accessed 24 July 2018] [Internet]. Available from:
https://www.acep.org/globalassets/uploads/uploaded-files/acep/membership/sections-of-
membership/ultra/workflow-white-paper.pdf
79. ACEP. Ultrasound Services in the Emergency Department. [policy statement]. Approved June 2022.
Available from: https://www.acep.org/patient-care/policy-statements/ultrasound-services-in-the-
emergency-department/
80. Byrne M, ACEP Emergency Ultrasound Section. Essential Machine Features [Internet]. 2014 [cited
2022 Apr 28]. Available from: https://www.acep.org/globalassets/uploads/uploaded-
files/acep/membership/sections-of-membership/ultra/essential-machine-features-2014.pdf
81. American College of Emergency Physicians. Appropriate Use Criteria for Handheld/Pocket
Ultrasound Devices [Internet]. 2018 [cited 2022 Apr 28]. Available from:
https://www.acep.org/globalassets/new-pdfs/policy-statements/appropriate-use-criteria-for-handheld-
ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 51 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
pocket-ultrasound-devices.pdf
82. Stolz L, O’Brien KM, Miller ML, Winters-Brown ND, Blaivas M, Adhikari S. A review of lawsuits
related to point-of-care emergency ultrasound applications. West J Emerg Med. 2015;16(1):1-4.
83. Labovitz AJ, Noble VE, Bierig M, et al. Focused cardiac ultrasound in the emergent setting: a
consensus statement of the American Society of Echocardiography and American College of
Emergency Physicians. J Am Soc Echocardiogr. 2010;23:1225-30.
84. Gaspari R, Dickman E. Effect of performing but not billing for emergency ultrasound in the
emergency department. Ann Emerg Med. 2005. 46(3s).S21.
85. Sierzenski PR, Fletcher S, O’Connor RE. 276: Emergency physicians who use ultrasound
demonstrate higher performance parameters compared to colleagues who are rare users, independent
of the clinical hours or shift type worked. Ann Emerg Med. 2007;50(3): Supplement S87.
86. Dean AJ, Zwank M, Strony R, Marin J. System Wide Clinical Ultrasound Resources. ACEP.
https://www.acep.org/emultrasound/subcommittees/system-wide-ultrasound-directors/
87. Philips Lumify. Accessed May 5, 2022, at https://www.usa.philips.com/healthcare/sites/lumify
88. EchoNous. Accessed May 5, 2022, at https://echonous.com/en_us/
89. GE Vscan Air. Accessed May 5, 2022, at
https://www.gehealthcare.com/products/ultrasound/handheld-ultrasound-vscan
90. Butterfly iQ+. Accessed May 5, 2022, at https://www.butterflynetwork.com/
91. EXO works. Accessed May 5, 2022, at https://www.exo.inc/
92. Hsieh A, Baker MB, Phalen JM, et al. Handheld point-of-care ultrasound: safety considerations for
creating guidelines. J Intensive Care Med. 2022;37(9):1146-51.
93. McGahan J, Pozniak, M, Cronan J, Pellerito J, Lee K, Blaivas, M. Handheld ultrasound: Threat or
opportunity? Appl Radiol. March 09, 2015.
94. ECRI. Top 10 health technology hazards for 2020: ECRI Institute. Accessed May 5, 2022, at
https://www.ecri.org/landing-2020-top-ten-health-technology-hazards
95. Marsh-Feiley G, Eadie L, Wilson P. Telesonography in emergency medicine: A systematic review.
PLoS One. 2018;13(5):e0194840.
96. Clinical Ultrasound Accreditation Program. http://www.cuap.org
97. Rubano, E, Mehta N, Caputo W, Paladino L, Sinert R. Systematic review: emergency department
bedside ultrasonography for diagnosing suspected abdominal aortic aneurysm Acad Emerg Med.
2013;20:128-38.
98. Mai T, Woo M, Boles K, Jetty P. Point of care ultrasound performed by a medical student compared
to physical examination by vascular surgeons in the detection of abdominal aortic aneurysms. Ann
Vasc Surg. 2018;52:15-21.
99. Guirguis-Blake JM, Beil TL, Senger CA, Coppola EL. Primary care screening for abdominal aortic
aneurysm: a systematic evidence review for the U.S. Preventive Services Task Force. Agency for
Healthcare Research and Quality (US), Rockville (MD); 2019.
100. Hoffmann B, Um P, Bessman ES, Ding R, Kelen GD, McCarthy ML. Routine screening for
asymptomatic abdominal aortic aneurysm in high-risk patients is not recommended in emergency
departments that are frequently crowded. Acad Emerg Med. 2009;16:1242-50.
101. Wang Y, Yu H, Cao Y, Wan Z. Early screening for aortic dissection with point-of-care ultrasound by
emergency physicians. J Ultrasound Med. 2020;39:1309-15.
102. Catalano O, Siani A. Ruptured abdominal aortic aneurysm. J Ultrasound Med. 2005;24:1077-83.
103. Nazerian P, Mueller C, Vanni S, et al. Integration of transthoracic focused cardiac ultrasound in the
diagnostic algorithm for suspected acute aortic syndromes. Eur Heart J. 2019;40(24):1952-60.
104. Sobczyk D, Nycz K. Feasibility and accuracy of bedside transthoracic echocardiography in diagnosis
of acute proximal aortic dissection. Cardiovasc Ultrasound. 2015;13:15.
105. Erbel R, Aboyans V, Boileau C, et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic
diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of
the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 52 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
Society of Cardiology (ESC) [published correction appears in Eur Heart J. 2015;1;36(41):2779.
106. Howell JM, Eddy OL, Lukens TW, et al. Clinical policy: Critical issues in the evaluation and
management of emergency department patients with suspected appendicitis. Ann Emerg Med.
2010;55(1):71-116.
107. Elikashvili I, Tay ET, Tsung JW. The effect of point-of-care ultrasonography on emergency
department length of stay and computed tomography utilization in children with suspected
appendicitis. Acad Emerg Med. 2014;21(2):163-70.
108. Gottlieb M, Peksa GD, Pandurangadu AV, Nakitende D, Takhar S, Seethala RR. Utilization of
ultrasound for the evaluation of small bowel obstruction: A systematic review and meta-analysis. Am
J Emerg Med. 2018;36(2):234-42.
109. Boniface KS, King JB, LeSaux MA, Haciski SC, Shokoohi H. Diagnostic accuracy and time-saving
effects of point-of-care ultrasonography in patients with small bowel obstruction: A prospective
study. Ann Emerg Med. 2020;75(2):246-56.
110. Laméris W, van Randen A, Bipat S, Bossuyt PM, Boermeester MA, Stoker J. Graded compression
ultrasonography and computed tomography in acute colonic diverticulitis: meta-analysis of test
accuracy. Eur Radiol. 2008;18(11):2498-511.
111. Cohen A, Li T, Stankard B, Nelson M. A prospective evaluation of point-of-care ultrasonographic
diagnosis of diverticulitis in the emergency department. Ann Emerg Med. 2020 Dec;76(6):757-
766.
112. Nazerian P, Gigli C, Donnarumma E, et al. Diagnostic accuracy of point-of-care ultrasound integrated
into clinical examination for acute diverticulitis: A prospective multicenter study. Ultraschall Med.
2021;42(6):614-22.
113. Yum J, Hoffman T, Naraghi L. Timely diagnosis of pneumoperitoneum by point-of-care ultrasound
in the emergency department: A case series. Clin Pract Cases Emerg Med. 2021;5(4):377-80.
114. Jiang L, Wu J, Feng X. The value of ultrasound in diagnosis of pneumoperitoneum in emergent or
critical conditions: A meta-analysis. Hong Kong J Emerg Med. 2019;26(2):111-7.
115. Robinson A, Light D, Nice C. Meta-analysis of sonography in the diagnosis of inguinal hernias. J
Ultrasound Med. 2013;32(2):339-46.
116. Siadecki SD, Frasure SE, Saul T, Lewiss RE. Diagnosis and reduction of a hernia by bedside
ultrasound: a case report. J Emerg Med. 2014;47(2):169-71.
117. Bergmann KR, Arroyo AC, Tessaro MO, et al. Diagnostic accuracy of point-of-care ultrasound for
intussusception: A multicenter, noninferiority study of paired diagnostic tests. Ann Emerg Med.
2021;78(5):606-15.
118. Lin-Martore M, Kornblith AE, Kohn MA, Gottlieb M. Diagnostic accuracy of point-of-care
ultrasound for intussusception in children presenting to the emergency department: A systematic
review and meta-analysis. West J Emerg Med. 2020;21(4):1008-16.
119. Kim JH, Lee JY, Kwon JH, Cho HR, Lee JS, Ryu JM. Point-of-care ultrasound could streamline the
emergency department workflow of clinically nonspecific intussusception. Pediatr Emerg Care.
2020;36(2):e90-e95.
120. Sivitz AB, Tejani C, Cohen SG. Evaluation of hypertrophic pyloric stenosis by pediatric emergency
physician sonography. Acad Emerg Med. 2013;20(7):646-51.
121. Park JS, Byun YH, Choi SJ, Lee JS, Ryu JM, Lee JY. Feasibility of point-of-care ultrasound for
diagnosing hypertrophic pyloric stenosis in the emergency department. Pediatr Emerg Care.
2021;37(11):550-4.
122. Gottlieb M, Alerhand S. Managing cardiac arrest using ultrasound [published online ahead of print,
2022 Nov 2]. Ann Emerg Med. 2022;S0196-0644(22)01120-9.
123. Mandavia D, Hoffner R, Mahaney K, et al. Bedside echocardiography by emergency physicians. Ann
Emerg Med. 2001;38:377-82.
124. Plummer D, Brunnette D, Asinger R,et al. Emergency department echocardiography improves
outcome in penetrating cardiac injury. Ann Emerg Med. 1992;21:709-12.

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 53 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
125. Inaba K, Chouliaras K, Zakaluzny, S, et al. FAST Ultrasound Examination as a Predictor of
Outcomes After Resuscitative Thoracotomy. Ann Surg. 2015;262(3):512-8.
126. Blaivas M, Fox J. Outcome in cardiac arrest patients found to have cardiac standstill on the bedside
emergency department echocardiogram. Acad Emerg Med. 2001;8:616-21.
127. Gaspari R, Weekes A, Adhikari S, et al. Emergency department point-of-care ultrasound in out-of-
hospital and in-ED cardiac arrest. Resuscitation. 2016;109:33-39.
128. Moore CL, Rose GA, Tayal VS, et al. Determination of left ventricular function by emergency
physician echocardiography of hypotensive patients. Acad Emerg Med. 2002;9(3):186-93.
129. Jones AE, Tayal VS, Sullivan DM, et al. Randomized, controlled trial of immediate versus delayed
goal-directed ultrasound to identify the cause of nontraumatic hypotension in emergency department
patients. Crit Care Med. 2004;32:1703-8.
130. Kanji HD, McCallum J, Sirounis D, et al. Limited echocardiography-guided therapy in subacute
shock is associated with change in management and improved outcomes. J Crit Care. 2014;29:700-5.
131. Nagdev AD, Merchant RC, Tirado-Gonzalez A, et al. Emergency department bedside
ultrasonographic measurement of the caval index for noninvasive determination of low central venous
pressure. Ann Emerg Med. 2010;55:290-5.
132. Perera P, Mailhot T, Riley D, et al. The RUSH exam: Rapid Ultrasound in SHock in the evaluation of
the critically ill. Emerg Med Clin North Am. 2010;28(1):29-56.
133. Russell FM, Ehrman RR, Cosby K, et al. Diagnosing acute heart failure in patients with
undifferentiated dyspnea: a lung and cardiac ultrasound (LuCUS) protocol. Acad Emerg Med.
2015;22:182-91.
134. Martindale JL, Wakai A, Collins SP, et al. Diagnosing acute heart failure in the emergency
department: A systematic review and meta-analysis. Acad Emerg Med. 2016;23(3):223-42.
135. Rutz MA, Clary JM, Kline JA, et al. Emergency physicians are able to detect right ventricular dilation
with good agreement compared to cardiology. Acad Emerg Med. 2017;24(7):867-74.
136. Fields JM, Davis J, Girson L, et al. Transthoracic echocardiography for diagnosing pulmonary
embolism: A systematic review and meta-analysis. JASE. 2017; 30(7):714-723.e4, 2017 Jul.
137. Weekes AJ, Thacker G, Troha D, et al. Diagnostic accuracy of right ventricular dysfunction markers
in normotensive emergency department patients with acute pulmonary embolism. Ann Emerg Med.
2016;68(3):277-91.
138. Weekes AJ, Raper JD, Lupez K, et al. Development and validation of a prognostic tool: Pulmonary
embolism short-term clinical outcomes risk estimation (PE-SCORE). PLoS One.
2021;16(11):e0260036.
139. Pomero F, Dentali F, Borretta V, Bonzini M, Melchio R, Douketis JD, Fenoglioet LM. Accuracy of
emergency physician-performed ultrasonography in the diagnosis of deep-vein thrombosis: A
systematic review and meta-analysis. Thromb Haemost. 2013;109:137-45.
140. Burnside PR, Brown MD, Kline JA. Systematic review of emergency physician-performed
ultrasonography for lower-extremity deep vein thrombosis. Acad Emerg Med. 2008;15:493-8.
141. Lee JH, Lee SH, Yun SJ. Comparison of 2-point and 3-point point-of-care ultrasound techniques for
deep vein thrombosis at the emergency department: A meta-analysis. Medicine (Baltimore).
2019;98(22):e15791.
142. Needleman L, Cronan JJ, Lilly MP, Merli GJ, Adhikari S, Hertzberg BS, DeJong MR, Streiff MB,
Meissner MH. Ultrasound for lower extremity deep venous thrombosis: multidisciplinary
recommendations from the Society of Radiologists in Ultrasound Consensus Conference. Circulation.
2018;137(14):1505-15.
143. Varrias D, Palaiodimos L, Balasubramanian P, et al. The use of point-of-care ultrasound (POCUS) in
the diagnosis of deep vein thrombosis. J Clin Med. 2021;10(17):3903.
144. Adhikari S, Zeger W, Thom C, Fields JM. Isolated deep venous thrombosis: implications for 2-point
compression ultrasonography of the lower extremity. Ann Emerg Med. 2015;66:262-6.
145. Frederick MG, Hertzberg BS, Kliewer MA, Paulson EK, Bowie JD, Lalouche KJ, DeLong DM,
ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 54 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
Carroll BA. Can the US examination for lower extremity deep venous thrombosis be abbreviated? A
prospective study of 755 examinations. Radiology. 1996;199:45-7.
146. Caronia J, Sarzynski A, Tofighi B, Mahdavi R-3. Resident performed two-point compression
ultrasound is inadequate for diagnosis of deep vein thrombosis in the critically ill. J Thromb
Thrombolysis. 2014;37:298-302.
147. Theodoro D, Blaivas M, Duggal S, et al. Real-time B-mode ultrasound in the ED saves time in the
diagnosis of deep vein thrombosis (DVT). Am J Emerg Med. 2004;22:197-200.
148. Oppenheimer DC, Rubens DJ. Sonography of acute cholecystitis and its mimics. Radiol Clin North
Am. 2019;57(3):535-48.
149. Blaivas M, Harwood RA, Lambert MJ. Decreasing length of stay with emergency department
gallbladder ultrasonography. Acad Emerg Med. 1999;6:541.
150. Villar J, Summers SM, Menchine MD, et al. The absence of gallstones on point-of-care ultrasound
rules out acute cholecystitis. J Emerg Med. 2015;49:475-80.
151. Kendall JL, Shimp RJ. Performance and interpretation of limited right upper quadrant ultrasound by
emergency physicians. J Emerg Med. 2001;21(1)7-13.
152. Miller AH, Pepe PE, Brockman CR, et al. ED ultrasound in hepatobiliary disease. J Emerg Med.
2006;30:69-74.
153. Ross M, Brown M, McLaughlin K, et al. Emergency physician-performed ultrasound to diagnose
cholelithiasis: a systematic review. Acad Emerg Med. 2011;18:227-35.
154. Summers SM, Scruggs W, Menchine MD, et al. A prospective evaluation of emergency department
bedside ultrasonography for the detection of acute cholecystitis. Ann Emerg Med. 2010;56:114-22.
155. Graglia S, Shokoohi H, Loesche MA, Yeh DD, Haney RM, Huang CK, Morone CC, Springer C,
Kimberly HH, Liteplo AS. Prospective validation of the bedside sonographic acute cholecystitis score
in emergency department patients. Am J Emerg Med. 2021;42:15-9.
156. Seyedhosseini J, Nasrelari A, Mohammadrezaei N, Karimialavijeh E. Inter-rater agreement between
trained emergency medicine residents and radiologists in the examination of gallbladder and common
bile duct by ultrasonography. Emerg Radiol. 2017;24(2):171-6.
157. Lahham S, Becker BA, Gari A, Bunch S, Alvarado M, Anderson CL, Viquez E, Spann SC, Fox JC.
Utility of common bile duct measurement in ED point of care ultrasound: A prospective study. Am J
Emerg Med. 2018;36(6):962-6.
158. Ripollés T, Martínez-Pérez MJ, Martin G, Vizuete J, Martínez-García R, Diez J, Martí E. Usefulness
of contrast-enhanced US in the diagnosis of acute gangrenous cholecystitis: A comparative study with
surgical and pathological findings. Eur J Radiol. 2016;85(1):31-8.
159. Secko MA, Reardon L, Gottlieb M, et al. Musculoskeletal ultrasonography to diagnose dislocated
shoulders: A prospective cohort. Ann Emerg Med. 2020;76(2):119-28.
160. Gottlieb M, Alerhand S. Ultrasound should be considered for all arthrocentesis. Ann Emerg Med.
2020;75(2):261-2.
161. Wu T, Dong Y, Song H, Fu Y, Li JH. Ultrasound-guided versus landmark in knee arthrocentesis: A
systematic review. Semin Arthritis Rheum. 2016;45(5):627-32.
162. Berona K, Abdi A, Menchine M, et al. Success of ultrasound-guided versus landmark-guided
arthrocentesis of hip, ankle, and wrist in a cadaver model. Am J Emerg Med. 2017;35(2):240-4.
163. Chartier LB, Bosco L, Lapointe-Shaw L, Chenkin J. Use of point-of-care ultrasound in long bone
fractures: a systematic review and meta-analysis. CJEM. 2017;19(2):131-42.
164. Gottlieb M, Cosby K. Ultrasound-guided hematoma block for distal radial and ulnar fractures. J
Emerg Med. 2015;48(3):310-2.
165. Bright JM, Fields KB, Draper R. Ultrasound diagnosis of calf injuries. Sports Health. 2017;9(4):352-
5.
166. Franks N, Gress J, Joseph R. Point-of-care ultrasound for suspected pectoralis major rupture: A case
report. Clin Pract Cases Emerg Med. 2021;5(1):93-6.
167. Schönberger TJ, Ernst MF. A brachialis muscle rupture diagnosed by ultrasound; case report. Int J

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 55 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
Emerg Med. 2011;4(1):46.
168. Situ-LaCasse E, Grieger RW, Crabbe S, Waterbrook AL, Friedman L, Adhikari S. Utility of point-of-
care musculoskeletal ultrasound in the evaluation of emergency department musculoskeletal
pathology. World J Emerg Med. 2018;9(4):262-6.
169. Connell DA, Schneider-Kolsky ME, Hoving JL, et al. Longitudinal study comparing sonographic and
MRI assessments of acute and healing hamstring injuries. AJR Am J Roentgenol. 2004;183:975-84.
170. Albayda J, van Alfen N. Diagnostic value of muscle ultrasound for myopathies and myositis. Curr
Rheumatol Rep. 2020;22(11):82.
171. Kumar MP, Seif D, Perera P, Mailhot T. Point-of-care ultrasound in diagnosing pyomyositis: a report
of three cases. J Emerg Med. 2014;47(4):420-6.
172. Bionat ED, Ongchuan MA. The utility of musculoskeletal ultrasonography in diagnosing
pyomyositis: a comparison with surgically and conservatively treated cases. J Diagn Med Sonogr.
2021;37(3):248-58.
173. Wu TS, Roque PJ, Green J, Drachman D, Khor KN, Rosenberg M, et al. Bedside ultrasound
evaluation of tendon injuries. Am J Emerg Med. 2012;30(8):1617-21.
174. Hubbard D, Joing S, Smith SW. Pyogenic flexor tenosynovitis by point-of-care ultrasound in the
emergency department. Clin Pract Cases Emerg Med. 2018;2(3):235-40.
175. Jardin E, Delord M, Aubry S, Loisel F, Obert L. Usefulness of ultrasound for the diagnosis of
pyogenic flexor tenosynovitis: A prospective single-center study of 57 cases. Hand Surg Rehabil.
2018;37(2):95-8.
176. Gottlieb M, Holladay D, Peksa GD. Point-of-care ocular ultrasound for the diagnosis of retinal
detachment: A systematic review and meta-analysis. Acad Emerg Med. 2019;26(8):931-9.
177. Lahham S, Shniter I, Thompson M, et al. Point-of-care ultrasonography in the diagnosis of retinal
detachment, vitreous hemorrhage, and vitreous detachment in the emergency department. JAMA Netw
Open. 2019;2(4):e192162.
178. Propst SL, Kirschner JM, Strachan CC, et al. Ocular point-of-care ultrasonography to diagnose
posterior chamber abnormalities: A systematic review and meta-analysis. JAMA Netw Open.
2020;3(2):e1921460.
179. Harries A, Shah S, Teismann N, Price D, Nagdev A. Ultrasound assessment of extraocular
movements and pupillary light reflex in ocular trauma. Am J Emerg Med. 2010 Oct;28(8):956-9.
180. Aletreby W, Alharthy A, Brindley PG, Kutsogiannis DJ, Faqihi F, Alzayer W, et al. Optic nerve
sheath diameter ultrasound for raised intracranial pressure: A literature review and meta-analysis of
its diagnostic accuracy. J Ultrasound Med. 2022;41(3):585-95.
181. Teismann N, Lenaghan P, Nolan R, Stein J, Green A. Point-of-care ocular ultrasound to detect optic
disc swelling. Acad Emerg Med. 2013;20(9):920-5.
182. Tayal VS, Cohen H, Norton HJ. Outcome of patients with an indeterminate emergency department
first-trimester pelvic ultrasound to rule out ectopic pregnancy. Acad Emerg Med. 2004;11(9):912-7.
183. Lewiss RE, Shaukat NM, Saul T. The endomyometrial thickness measurement for abnormal
implantation evaluation by pelvic sonography. J Ultrasound Med. 2014 Jul;33(7):1143-6.
184. Wang R, Reynolds TA, West HH, Ravikumar D, Martinez C, McAlpine I, Jacoby VL, Stein JC.
Use of a β-hCG discriminatory zone with bedside pelvic ultrasonography. Ann Emerg Med.
2011;58(1):12-20.
185. Stone BS, Muruganandan KM, Tonelli MM, Dugas JN, Verriet IE, Pare JR. Impact of point-of-care
ultrasound on treatment time for ectopic pregnancy. Am J Emerg Med. 2021 Nov;49:226-32.
186. Moore C, Todd WM, O'Brien E, Lin H. Free fluid in Morison's pouch on bedside ultrasound predicts
need for operative intervention in suspected ectopic pregnancy. Acad Emerg Med. 2007
Aug;14(8):755-8.
187. Stein JC, Wang R, Adler N, Boscardin J, Jacoby VL, Won G, Goldstein R, Kohn MA. Emergency
physician ultrasonography for evaluating patients at risk for ectopic pregnancy: a meta-analysis. Ann
Emerg Med. 2010;56(6):674-83.
ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 56 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
188. Saul T, Lewiss RE, Rivera Mdel R. Accuracy of emergency physician performed bedside ultrasound
in determining gestational age in first trimester pregnancy. Crit Ultrasound J. 2012;4(1):22.
189. Beals T, Naraghi L, Grossestreuer A, Schafer J, Balk D, Hoffmann B. Point of care ultrasound is
associated with decreased ED length of stay for symptomatic early pregnancy. Am J Emerg Med.
2019;37(6):1165-8.
190. Berzon B, Gleenberg M, Offenbacher J, West D. Atypical presentation of hemorrhagic shock in
pregnancy: a case highlighting the developing field of emergency medicine in Israel. BMC Emerg
Med. 2019;19(1):70. Erratum in: BMC Emerg Med. 2020;20(1):4.
191. Derr C, Henry M. Bedside ultrasound in the diagnosis of uterine rupture following surgical abortion.
Emerg Radiol. 2013;20(2):165-7.
192. Wiese KS, Ernest S, Dukes WS. Case report of traumatic uterine rupture in a multigravida woman
with emergency department cesarean section. Clin Pract Cases Emerg Med. 2020;4(4):623-5.
193. Adkins K, Minardi J, Setzer E, Williams D. Retained products of conception: An atypical
presentation diagnosed immediately with bedside emergency ultrasound. Case Rep Emerg Med.
2016;2016:9124967.
194. Brass P, Hellmich M, Kolodziej L, Schick G, Smith AF. Ultrasound guidance versus anatomical
landmarks for internal jugular vein catheterization. Cochrane Database Syst Rev.
2015;1(1):CD006962.
195. Brass P, Hellmich M, Kolodziej L, Schick G, Smith AF. Ultrasound guidance versus anatomical
landmarks for subclavian or femoral vein catheterization. Cochrane Database Syst Rev.
2015;1(1):CD011447.
196. Agency for Healthcare Research and Quality. Evidence Report/Technology Assessment: Number 43.
Making Health Care Safer. A Critical Analysis of Patient Safety Practices: Summary. Accessed
January 2, 2023. Available at: http://archive.ahrq.gov/clinic/ptsafety/pdf/ptsafety.pdf.
197. Cattau EL Jr, Benjamin SB, Knuff TE, Castell DO. The accuracy of the physical examination in the
diagnosis of suspected ascites. JAMA. 1982;247(8):1164-6.
198. Nazeer SR, Dewbre H, Miller AH. Ultrasound-assisted paracentesis performed by emergency
physicians vs the traditional technique: a prospective, randomized study. Am J Emerg Med.
2005;23(3):363-7.
199. Mercaldi CJ, Lanes SF. Ultrasound guidance decreases complications and improves the cost of care
among patients undergoing thoracentesis and paracentesis. Chest. 2013;143(2):532-8.
200. Patel PA, Ernst FR, Gunnarsson CL. Ultrasonography guidance reduces complications and costs
associated with thoracentesis procedures. J Clin Ultrasound. 2012;40(3):135-41.
201. Gordon CE, Feller-Kopman D, Balk EM, Smetana GW. Pneumothorax following thoracentesis: a
systematic review and meta-analysis. Arch Intern Med. 2010;170(4):332-9.
202. Costantino TG, Satz WA, Dehnkamp W, Goett H. Randomized trial comparing intraoral ultrasound to
landmark-based needle aspiration in patients with suspected peritonsillar abscess. Acad Emerg Med.
2012;19(6):626-31.
203. Tsang TS, Enriquez-Sarano M, Freeman WK, Barnes ME, Sinak LJ, Gersh BJ, Bailey KR, Seward
JB. Consecutive 1127 therapeutic echocardiographically guided pericardiocenteses: clinical profile,
practice patterns, and outcomes spanning 21 years. Mayo Clin Proc. 2002;77(5):429-36.
204. Lindenberger M, Kjellberg M, Karlsson E, Wranne B. Pericardiocentesis guided by 2-D
echocardiography: the method of choice for treatment of pericardial effusion. J Intern Med.
2003;253(4):411-7.
205. Gottlieb M, Avila J, Chottiner M, Peksa GD. Point-of-care ultrasonography for the diagnosis of skin
and soft tissue abscesses: A systematic review and meta-analysis. Ann Emerg Med. 2020;76(1):67-77.
206. Marin JR, Dean AJ, Bilker WB, Panebianco NL, Brown NJ, Alpern ER. Emergency ultrasound-
assisted examination of skin and soft tissue infections in the pediatric emergency department. Acad
Emerg Med. 2013;20(6):545-53.
207. Schmitz GR, Gottlieb M. Managing a cutaneous abscess in the emergency department. Ann Emerg
ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 57 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
Med. 2021;78(1):44-8.
208. Davis J, Czerniski B, Au A, Adhikari S, Farrell I, Fields JM. Diagnostic Accuracy of
Ultrasonography in Retained Soft Tissue Foreign Bodies: A Systematic Review and Meta-analysis.
Acad Emerg Med. 2015;22(7):777-87.
209. Lahham S, Shniter I, Desai M, Andary R, Saadat S, Fox JC, Pierce S. Point of care ultrasound in the
diagnosis of necrotizing fasciitis. Am J Emerg Med. 2022;51:397-400.
210. Yen Z, Wang H, Ma H, Chen S, Chen W. Ultrasonographic screening of clinically-suspected
necrotizing fasciitis. Acad Emerg Med. 2002;9(12):1448-51.
211. Wright S, Hoffmann B. Emergency ultrasound of acute scrotal pain. Eur J Emerg Med. 2015;22(1):2-
9.
212. Ramanathan S, Bertolotto M, Freeman S, et al. Imaging in scrotal trauma: a European Society of
Urogenital Radiology Scrotal and Penile Imaging Working Group (ESUR-SPIWG) position
statement. Eur Radiol. 2021;31:4918-28.
213. Ota K, Fukui K, Oba K, et al. The role of ultrasound imaging in adult patients with testicular torsion:
a systematic review and meta-analysis. J Med Ultrasonics. 2019;46:325-34.
214. Liang T, Metcalfe P, Sevcik W, Noga M. Retrospective review of diagnosis and treatment in children
presenting to the pediatric department with acute scrotum. AJR Am J Roentgenol. 2013;200:5.
215. Blaivas M, Sierzenski P. Emergency ultrasonography in the evaluation of the acute scrotum. Acad
Emerg Med. 2001;8(1):85-9.
216. Blaivas M, Sierzenski P, Lambert M. Emergency evaluation of patients presenting with acute scrotum
using bedside ultrasonography. Acad Emerg Med. 2001;8(1):90-3.
217. Friedman N, Pancer Z, Savic R, Tseng F, Lee MS, Mclean L, Bagli DJ, Tessaro MO. Accuracy of
point-of-care ultrasound by pediatric emergency physicians for testicular torsion. J Pediatr Urol.
2019;15(6):608.e1-608.e6.
218. McDowall J, Adam A, Gerber L, et al. The ultrasonographic “whirlpool sign” in testicular torsion:
valuable tool or waste of valuable time? A systematic review and meta-analysis. Emerg Radiol.
2018;25:281-92.
219. Morrison D, Blaivas M, Lyon M. Emergency diagnosis of Fournier's gangrene with bedside
ultrasound. Am J Emerg Med. 2005;23(4):544-7.
220. Sadjo SA, Destinval C, Lemelle JL, Berte N. Testicular rupture after blunt scrotal trauma in children:
A case report and literature review. Trauma Case Rep. 2021;33:100482.
221. McGivery K, Atkinson P, Lewis D, et al. Emergency department ultrasound for the detection of B-
lines in the early diagnosis of acute decompensated heart failure: a systematic review and meta-
analysis. CJEM. 2018;20(3):343-52.
222. Orso D, Guglielmo N, Copetti R. Lung ultrasound in diagnosing pneumonia in the emergency
department: a systematic review and meta-analysis. Eur J Emerg Med. 2018;25(5):312-21.
223. Alzahrani SA, Al-Salamah MA, Al-Madani WH, et al. Systematic review and meta-analysis for the
use of ultrasound versus radiology in diagnosing of pneumonia. Crit Ultrasound J. 2017;9(1):6.
224. Lu X, Jin Y, Li Y, et al. Diagnostic accuracy of lung ultrasonography in childhood pneumonia: a
meta-analysis. Eur J Emerg Med. 2022;29(2):105-17.
225. Pereda MA, Chavez MA, Hooper-Miele CC, et al. Lung ultrasound for the diagnosis of pneumonia in
children: a meta-analysis. Pediatrics. 2015;135(4):714-22.
226. Gil-Rodriguez J, de Rojas JP, Aranda-Laserna P, et al. Ultrasound findings of lung ultrasonography in
COVID-19: A systematic review. Eur J Radiol. 2022;148:110156.
227. Hosseini M, Ghelichkhani P, Baikpour M, et al. Diagnostic accuracy of ultrasonography and
radiography in detection of pulmonary contusion; a systematic review and meta-Analysis. Emerg
(Tehran). 2015;3(4):127-36.
228. Hansell L, Milross M, Delaney A, et al. Lung ultrasound has greater accuracy than conventional
respiratory assessment tools for the diagnosis of pleural effusion, lung consolidation and collapse: a
systematic review. J Physiother. 2021;67(1):41-8.

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 58 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
229. Zare MA, Bahmani A, Fathi M, et al. Role of point-of-care ultrasound study in early disposition of
patients with undifferentiated acute dyspnea in emergency department: a multi-center prospective
study. J Ultrasound. 2022;25(3):443-9.
230. Gottlieb M, Holladay D, Burns KM, Nakitende D, Bailitz J. Ultrasound for airway management: An
evidence-based review for the emergency clinician. Am J Emerg Med. 2020;38(5):1007-13.
231. Adhikari S, Zeger W, Schmier C, et al. Pilot study to determine the utility of point-of-care ultrasound
in the assessment of difficult laryngoscopy. Acad Emerg Med. 2011;18(7):754-8.
232. Gottlieb M, Holladay D, Peksa GD. Ultrasonography for the Confirmation of Endotracheal Tube
Intubation: A Systematic Review and Meta-Analysis. Ann Emerg Med. 2018;72(6):627-36.
233. Gottlieb M, Holladay D, Serici A, Shah S, Nakitende D. Comparison of color flow with standard
ultrasound for the detection of endotracheal intubation. Am J Emerg Med. 2018;36(7):1166-9.
234. Gottlieb M, Nakitende D, Sundaram T, Serici A, Shah S, Bailitz J. Comparison of Static versus
Dynamic Ultrasound for the Detection of Endotracheal Intubation. West J Emerg Med.
2018;19(2):412-6.
235. Gottlieb M, Holladay D, Burns K, et al. Accuracy of ultrasound for endotracheal intubation between
different transducer types. Am J Emerg Med. 2019;37(12):2182-5.
236. Gottlieb M, Holladay D, Nakitende D, et al. Variation in the accuracy of ultrasound for the detection
of intubation by endotracheal tube size. Am J Emerg Med. 2019;37(4):706-9.
237. Gottlieb M, Burns K, Holladay D, Chottiner M, Shah S, Gore SR. Impact of endotracheal tube
twisting on the diagnostic accuracy of ultrasound for intubation confirmation. Am J Emerg Med.
2020;38(7):1332-4.
238. Gottlieb M, Alerhand S, Long B. Point-of-Care Ultrasound for Intubation Confirmation of COVID-
19 Patients. West J Emerg Med. 2020;21(5):1042-5.
239. Gottlieb M, Patel D, Sundaram T. Comparison of endotracheal tube location on ultrasound accuracy,
time, and confidence. Am J Emerg Med. 2022 Dec;62:127-128.
240. Link MS, Berkow LC, Kudenchuk PJ, et al. Part 7: Adult Advanced Cardiovascular Life Support:
2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and
Emergency Cardiovascular Care. Circulation. 2015;132(18 Suppl 2):S444-S464.
241. Mallin M, Curtis K, Dawson M, Ockerse P, Ahern M. Accuracy of ultrasound-guided marking of the
cricothyroid membrane before simulated failed intubation. Am J Emerg Med. 2014;32(1):61-3.
242. Siddiqui N, Yu E, Boulis S, You-Ten KE. Ultrasound Is Superior to Palpation in Identifying the
Cricothyroid Membrane in Subjects with Poorly Defined Neck Landmarks: A Randomized Clinical
Trial. Anesthesiology. 2018;129(6):1132-9.
243. Curtis K, Ahern M, Dawson M, Mallin M. Ultrasound-guided, Bougie-assisted cricothyroidotomy: a
description of a novel technique in cadaveric models. Acad Emerg Med. 2012;19(7):876-9.
244. ATLS Subcommittee; American College of Surgeons’ Committee on Trauma; International ATLS
working group. Advanced trauma life support (ATLS®): the ninth edition. J Trauma Acute Care
Surg. 2013;74(5):1363-6.
245. Pearl WS, Todd KH. Ultrasonography for the initial evaluation of blunt abdominal trauma: A review
of prospective trials. Ann Emerg Med. 1996;27(3):353-61.
246. American Institute of Ultrasound in Medicine; American College of Emergency Physicians. AIUM
practice guideline for the performance of the focused assessment with sonography for trauma (FAST)
examination. J Ultrasound Med. 2014;33(11):2047-56. Accessed December 2022 at:
https://www.aium.org/resources/guidelines/fast.pdf
247. Jahanshir A, Moghari SM, Ahmadi A, Moghadam PZ, Bahreini M. Value of point-of-care
ultrasonography compared with computed tomography scan in detecting potential life-threatening
conditions in blunt chest trauma patients. Ultrasound J. 2020;12(1):36.
248. Volpicelli G, Elbarbary M, Blaivas M, et al. International evidence-based recommendations for point-
of-care lung ultrasound. Intensive Care Med. 2012;38:577-91.
249. Governatori NJ, Saul T, Siadecki SD, Lewiss RE. Ultrasound in the evaluation of penetrating
ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 59 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
thoraco-abdominal trauma: a review of the literature. Med Ultrason. 2015;17(4):528-34.
250. Melniker LA, Leibner E, McKenney MG, Lopez P, Briggs WM, Mancuso CA. Randomized
controlled clinical trial of point-of-care, limited ultrasonography for trauma in the emergency
department: the first sonography outcomes assessment program trial. Ann Emerg Med.
2006;48(3):227-35.
251. Sheng AY, Dalziel P, Liteplo AS, et al. Focused assessment with sonography in trauma and
abdominal computed tomography utilization in adult trauma patients: Trends over the last decade.
Emerg Med Int. 2013;2013:678380.
252. American College of Emergency Physicians. Ultrasound Guided Nerve Blocks [policy statement].
Approved April 2021. Accessed November 18, 2022. Available from:
https://www.acep.org/globalassets/new-pdfs/policy-statements/ultrasound-guided-nerve-blocks.pdf
253. Welch MB, Brummett CM, Welch TD, Tremper KK, Shanks AM, Guglani P, Mashour GA.
Perioperative peripheral nerve injuries: a retrospective study of 380,680 cases during a 10-year period
at a single institution. Anesthesiology. 2009;111(3):490-7.
254. Sites BD, Barrington MJ, Davis M. Using an international clinical registry of regional anesthesia to
identify targets for quality improvement. Reg Anesth Pain Med. 2014;39(6):487-95.
255. Raeyat Doost E, Heiran MM, Movahedi M, Mirafzal A. Ultrasound-guided interscalene nerve block
vs procedural sedation by propofol and fentanyl for anterior shoulder dislocations. Am J Emerg Med.
2017;35(10):1435-9.
256. Abdelhamid K, ElHawary H, Turner JP. The use of the erector spinae plane block to decrease pain
and opioid consumption in the emergency department: A literature review. J Emerg Med.
2020;58(4):603-9.
257. Tekşen Ş, Öksüz G, Öksüz H, Sayan M, Arslan M, Urfalıoğlu A, Gişi G, Bilal B. Analgesic efficacy
of the serratus anterior plane block in rib fractures pain: A randomized controlled trial. Am J Emerg
Med. 2021;41:16-20.
258. Surdhar I, Jelic T. The erector spinae plane block for acute pain management in emergency
department patients with rib fractures. CJEM. 2022;24(1):50-4.
259. Aydin ME, Tekin E, Ahiskalioglu EO, Ates I, Karagoz S, Aydin OF, Ozkaya F, Ahiskalioglu A.
Erector spinae plane block vs non-steroidal anti-inflammatory drugs for severe renal colic pain: A
pilot clinical feasibility study. Int J Clin Pract. 2021;75(3):e13789.
260. Herring AA, Stone MB, Nagdev AD. Ultrasound-guided abdominal wall nerve blocks in the ED. Am
J Emerg Med. 2012;30(5):759-64.
261. Mahmoud S, Miraflor E, Martin D, Mantuani D, Luftig J, Nagdev AD. Ultrasound-guided transverse
abdominis plane block for ED appendicitis pain control. Am J Emerg Med. 2019;37(4):740-3.
262. Brox WT, Roberts KC, Taksali S, Wright DG, Wixted JJ, Tubb CC, et al. The American Academy of
Orthopaedic Surgeons Evidence-Based Guideline on Management of Hip Fractures in the Elderly. J
Bone Joint Surg Am. 2015;97(14):1196-9.
263. American College of Surgeons. Best practices guidelines for acute pain management in trauma
patients. November 2020. Available at: https://www.facs.org/-/media/files/quality-
programs/trauma/tqip/acute_pain_guidelines.ashx
264. Guay J, Kopp S. Peripheral nerve blocks for hip fractures in adults. Cochrane Database Syst Rev.
2020 Nov 25;11(11):CD001159.
265. Kolodychuk N, Krebs JC, Stenberg R, Talmage L, Meehan A, DiNicola N. Fascia iliaca blocks
performed in the emergency department decrease opioid consumption and length of stay in patients
with hip fracture. J Orthop Trauma. 2022;36(3):142-6.
266. Makkar JK, Singh NP, Bhatia N, Samra T, Singh PM. Fascia iliaca block for hip fractures in the
emergency department: meta-analysis with trial sequential analysis. Am J Emerg Med. 2021;50:654-
60.
267. Luftig J, Dreyfuss A, Mantuani D, Howell K, White A, Nagdev A. A new frontier in pelvic fracture
pain control in the ED: Successful use of the pericapsular nerve group (PENG) block. Am J Emerg

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 60 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
Med. 2020;38(12):2761.e5-2761.e9.
268. Goldsmith AJ, Liteplo A, Hayes BD, Duggan N, Huang C, Shokoohi H. Ultrasound-guided
transgluteal sciatic nerve analgesia for refractory back pain in the ED. Am J Emerg Med.
2020;38(9):1792-5.
269. Cisewski DH, Alerhand S. 'SCALD-ED' Block: Superficial Cutaneous Anesthesia in a Lateral Leg
Distribution within the Emergency Department - A Case Series. J Emerg Med. 2019;56(3):282-7.
270. Vrablik M, Akhavan A, Murphy D, Schrepel C, Hall MK. Ultrasound-guided nerve blocks for painful
hand injuries: A randomized control trial. Cureus. 2021;13(10):e18978.
271. Moore CL, Carpenter CR, Heilbrun ME, et al. Imaging in suspected renal colic: systematic review of
the literature and multispecialty consensus. Ann Emerg Med. 2019;74(3):391-9.
272. Park YH, Jung RB, Lee YG, et al. Does the use of bedside ultrasonography reduce emergency
department length of stay for patients with renal colic?: a pilot study. Clin Exp Emerg Med.
2016;3(4):197-203.
273. Wong C, Teitge B, Ross M, Young P, Robertson HL, Lang E. The accuracy and prognostic value of
point-of-care ultrasound for nephrolithiasis in the emergency department: A systematic review and
meta-analysis. Acad Emerg Med. 2018;25(6):684-98.
274. Smith-Bindman R, Aubin C, Bailitz J, et al. Ultrasonography versus computed tomography for
suspected nephrolithiasis. N Engl J Med. 2014;371:1100-10.
275. Herbst MK, Rosenberg G, Daniels B, et al. Effect of provider experience on clinician-performed
ultrasonography for hydronephrosis in patients with suspected renal colic. Ann Emerg Med.
2014;64(3):269-76.
276. Daniels B, Gross CP, Molinaro A, et al. STONE PLUS: Evaluation of emergency department patients
with suspected renal colic, using a clinical prediction tool combined with point-of-care limited
ultrasonography. Ann Emerg Med. 2016;67(4):439-48.
277. Witt M, Baumann BM, McCans K. Bladder ultrasound increases catheterization success in pediatric
patients. Acad Emerg Med. 2005;12(4):371-4.
278. Lambert MJ, Villa M. Gynecologic ultrasound in emergency medicine. Emerg Med Clin North Am.
2004;22(3):683-96.
279. Tayal VS, Crean CA, Norton HJ, Schulz CJ, Bacalis KN, Bliss S. Prospective comparative trial of
endovaginal sonographic bimanual examination versus traditional digital bimanual examination in
nonpregnant women with lower abdominal pain with regard to body mass index classification. J
Ultrasound Med. 2008;27(8):1171-7.
280. Houry D, Abbott JT. Ovarian torsion: a fifteen-year review. Ann Emerg Med. 2001;38(2):156-9.
281. Johnson S, Fox JC, Koenig KL. Diagnosis of ovarian torsion in a hemodynamically unstable pediatric
patient by bedside ultrasound in the ED. Am J Emerg Med. 2006;24(4):496-7.
282. Lee DC, Swaminathan AK. Sensitivity of ultrasound for the diagnosis of tubo-ovarian abscess: a case
report and literature review. J Emerg Med. 2011;40(2):170-5.
283. Adhikari S, Blaivas M, Lyon M. Role of bedside transvaginal ultrasonography in the diagnosis of
tubo-ovarian abscess in the emergency department. J Emerg Med. 2008;34(4):429-33.
284. Bellapu S, Guttman J. Use of point-of-care ultrasound for the diagnosis of ovarian hyperstimulation
syndrome. J Emerg Med. 2017;52(4):e101-e104.
285. Hall MK, Coffey EC, Herbst M, Liu R, Pare JR, Taylor RA, Thomas S, Moore CL. The 5Es of
emergency physician-performed focused cardiac ultrasound: a protocol for rapid identification of
effusion, ejection, equality, exit and entrance. Acad Emerg Med. 2015;22(5):583-93.
286. Alerhand S, Adrian RJ, Long B, Avila J. Pericardial tamponade: A comprehensive emergency
medicine and echocardiography review. Am J Emerg Med. 2022;58:159-74.
287. Ehrman RR, Russel FM, Ansari AH, Margeta B, Clary JM, Christian E, Cosby KS, Bailitz J. Can
emergency physicians diagnose and correctly classify diastolic dysfunction using bedside
echocardiography? Am J Emerg Med. 2015;33(9):1178-83.
288. Del Rios M, Colla J, Kotini-Shah P, Briller J, Gerber B, Prendergast H. Emergency physician use of

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 61 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
tissue Doppler bedside echocardiography in detecting diastolic dysfunction: an exploratory study.
Crit Ultrasound J. 2018;10(1):4.
289. Alerhand S, Sundaram T, Gottlieb M. What are the echocardiographic findings of acute right
ventricular strain that suggest pulmonary embolism? Anaesth Crit Care Pain Med.
2021;40(2):100852.
290. Daley J, Grotberg J, Pare J, Medoro A, Liu R, Hall MK, Taylor A, Moore CL. Emergency physician
performed tricuspid annular plane systolic excursion in the evaluation of suspected pulmonary
embolism. Am J Emerg Med. 2017;35(1):106-11.
291. Shah BR, Velamakanni WM, Patel A, Khadkikar G, Patel TM, Shah SC. Analysis of the 60/60 sign
and other right ventricular parameters by 2D transthoracic echocardiography as adjuncts to diagnosis
of acute pulmonary embolism. Cureus. 2021;13(3): e13800.
292. Croft PE, Strout TD, Kring RM, Director L, Vasaiwala SC, Mackenzie DC. WAMAMI: emergency
physicians can accurately identify wall motion abnormalities in acute myocardial infarction. Am J
Emerg Med. 2019;37(12): 2224-8.
293. Saglam C, Unluer EE, Yamanoglu NGC, Kara PH, Ediboglu E, Bektasli R, Tandon S, Gonulu H.
Accuracy of emergency physicians for detection of regional wall motion abnormalities in patients
with chest pain without ST-elevation myocardial infarction. J Ultrasound Med. 2021;40(7):1335-42.
294. Dinh VA, Ko HS, Rao R, Bansal RC, Smith DD, Kin TE, Nguyen HB. Measuring cardiac index with
a focused cardiac ultrasound examination in the ED. Am J Emerg Med. 2012;30(9):1845-51.
295. MacKenzie DC, Khan NA, Blehar D, Glazier S, Chang Y, Stowell CP, Noble VE, Liteplo AS.
Carotid flow time changes with volume status in acute blood loss. Ann Emerg Med. 2015;66(3):277-
282.
296. Hu K, Gupta N, Teran F, Saul T, Nelson BP, Andrus P. Variability in interpretation of cardiac
standstill among physician sonographers. Ann Emerg Med. 2018;71(2):193-8.
297. Clattenburg EJ, Wroe PC, Gardner K, Schultz C, Gelber J, Singh A, Nagdev A. Implementation of
the cardiac arrest sonographic assessment (CASA) protocol for patients with cardiac arrest is
associated with shorter CPR pulse checks. Resuscitation. 2018;131:69-73.
298. Liu RB, Bogucki S, Marcolini EG, Yu CY, Wira CR, Kalam S, Daley J, Moore CL, Cone DC.
Guiding cardiopulmonary resuscitation with focused echocardiography: a report of five cases.
Prehosp Emerg Care. 2020;24(2): 297-302.
299. Gaspari R, Weekes A, Adhikari S, Noble V, Nomura JT, Theodoro D, et al. A retrospective study of
pulseless electrical activity, bedside ultrasound identifies interventions during resuscitation associated
with improved survival to hospital admission. A REASON study. Resuscitation. 2017;120:103-7.
300. Kummer T, Oh L, Phelan MB, Huang RD, Nomura JT, Adhikari S. Emergency and critical care
applications for contrast-enhanced ultrasound. Am J Emerg Med. 2018;36(7):1287-94.
301. Catalano O, Aiani L, Barozzi L, Bokor D, De Marchi A, Faletti C, et al. CEUS in abdominal trauma:
multi-center study. Abdom Imaging. 2009;34(2):225-34.
302. Tang C, Fang K, Guo Y, Li R, Fan X, Chen P, et al. Safety of sulfur hexafluoride microbubbles in
sonography of abdominal and superficial organs: retrospective analysis of 30,222 cases. J Ultrasound
Med. 2017;36(3):531-8.
303. Catalano O, Lobianco R, Cusati B, Siani A. Contrast-enhanced sonography for diagnosis of ruptured
abdominal aortic aneurysm. AJR Am J Roentgenol. 2005;184(2):423-7.
304. El Kadi S, Porter TR, Verouden N, van Rossum A, Kamp O. Contrast ultrasound, sonothrombolysis
and sonoperfusion in cardiovascular disease: shifting to theragnostic clinical trials. JACC Cardiovasc
Imaging. 2021 Oct 7;S1936-878X(21)00689-6.
305. Emanuel A, Meijer R, Poelgeest E, Spoor P, Serne E, Eringa E. Contrast-enhanced ultrasound for
quantification of tissue perfusion in humans. Microcirculation. 2020;27(1):e12588.
306. Hakim SM, Abdellatif AA, Ali MI, Ammar MA. Reliability of transcranial sonography for
assessment of brain midline shift in adult neurocritical patients: a systematic review and meta-
analysis. Minerva Anestesiol. 2021;87(4):467-75.

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 62 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
307. Kumar G, Shahripour RB, Harrigan MR. Vasospasm on transcranial Doppler is predictive of delayed
cerebral ischemia in aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. J
Neurosurg. 2016;124(5):1257-64.
308. Zhang XH, Liang HM. Systematic review with network meta-analysis: Diagnostic values of
ultrasonography, computed tomography, and magnetic resonance imaging in patients with ischemic
stroke. Medicine (Baltimore). 2019;98(30):e16360.
309. Fernando SM, Tran A, Cheng W, et al. Diagnosis of elevated intracranial pressure in critically ill
adults: systematic review and meta-analysis. BMJ. 2019;366:l4225.
310. Chang JJ, Tsivgoulis G, Katsanos AH, Malkoff MD, Alexandrov AV. Diagnostic Accuracy of
Transcranial Doppler for Brain Death Confirmation: Systematic Review and Meta-Analysis. AJNR
Am J Neuroradiol. 2016;37(3):408-14.
311. van der Wouw PA, Koster RW, Delemarre BJ, et al. Diagnostic accuracy of transesophageal
echocardiography during cardiopulmonary resuscitation. J Am Coll Cardiol. 1997;30(3):780-3.
312. Varriale P, Maldonado JM. Echocardiographic observations during in hospital cardiopulmonary
resuscitation. Crit Care Med. 1997;25(10):1717-20.
313. Miyake M, Izumi C, Takahashi S, et al. Efficacy of transesophageal echocardiography in patients
with cardiac arrest or shock. J Cardiol. 2004;44(5):189-94.
314. Memtsoudis SG, Rosenberger P, Loffler M, et al. The usefulness of transesophageal
echocardiography during intraoperative cardiac arrest in noncardiac surgery. Anesth Analg.
2006;102(6):1653-7.
315. Lin T, Chen Y, Lu C, et al. Use of transoesophageal echocardiography during cardiac arrest in
patients undergoing elective non-cardiac surgery. Br J Anaesth. 2006;96(2):167-70.
316. Shillcutt SK, Markin NW, Montzingo CR, et al. Use of rapid "rescue" perioperative
echocardiography to improve outcomes after hemodynamic instability in noncardiac surgical patients.
J Cardiothorac Vasc Anesth. 2012;26(3):362-70.
317. Hilberath JN, Burrage PS, Shernan SK, et al. Rescue transoesophageal echocardiography for
refractory haemodynamic instability during transvenous lead extraction. Eur Heart J Cardiovasc
Imaging. 2014;15(8):926-32.
318. Arntfield R, Pace J, Hewak M, Thompson D. Focused transesophageal echocardiography by
emergency physicians is feasible and clinically influential: observational results from a novel
ultrasound program. J Emerg Med. 2016;50(2):286-94.
319. Reardon RF, Chinn E, Plummer D, et al. Feasibility, utility, and safety of fully incorporating
transesophageal echocardiography into emergency medicine practice. Acad Emerg Med.
2022;29(3):334-43.
320. Hwang SO, Zhao PG, Choi HJ, et al. Compression of the left ventricular outflow tract during
cardiopulmonary resuscitation. Acad Emerg Med. 2009;16(10):928-33.
321. Cha KC, Kim YJ, Shin HJ, et al. Optimal position for external chest compression during
cardiopulmonary resuscitation: an analysis based on chest CT in patients resuscitated from cardiac
arrest. Emerg Med J. 2013;30(8):615-9.
322. Teran F, Dean AJ, Centeno C, et al.; Evaluation of out-of-hospital cardiac arrest using
transesophageal echocardiography in the emergency department. Resuscitation. 2019;137:140-7.
323. Catena E, Ottolina D, Fossali T, et al. Association between left ventricular outflow tract opening and
successful resuscitation after cardiac arrest. Resuscitation. 2019;138:8-14.
324. Fair J 3rd, Mallin MP, Adler A, et al. Transesophageal echocardiography during cardiopulmonary
resuscitation is associated with shorter compression pauses compared with transthoracic
echocardiography. Ann Emerg Med. 2019;73(6):610-6.
325. Lerner RP, Haaland A, Lin J. Temporary transvenous pacer placement under transesophageal
echocardiogram guidance in the Emergency Department. Am J Emerg Med. 2020;38(5):1044.e3-
1044.e4.
326. Fair J, Tonna J, Ockerse P. Emergency physician-performed transesophageal echocardiography for

ACEP
POLICY
STATEMENT
Ultrasound Guidelines: Emergency, Point-of-care, and
Clinical Ultrasound Guidelines in Medicine
Page 63 of 63
Copyright © 2023 American College of Emergency Physicians. All rights reserved.
American College of Emergency Physicians ● PO Box 619911 ● Dallas, TX 75261-9911 ● 972-550-0911 ● 800-798-1822
extracorporeal life support vascular cannula placement. Am J Emerg Med. 2016; 34(8):1637-9.
327. Teran F, Abella B. (2021, July - ). Resuscitative TEE collaborative registry (rTEECoRe). Identifier
NCT04972526. https://www.clinicaltrials.gov/ct2/show/NCT04972526
